No, amoxicillin doesn’t directly stain teeth yellow. However, certain factors related to its use or underlying health conditions can lead to discoloration. This discoloration isn’t permanent in most cases and often resolves with proper dental hygiene and addressing potential contributing causes.
Tetracycline antibiotics, not amoxicillin, are the primary culprits for causing permanent yellowing or staining of teeth, especially in children whose teeth are still developing. If you suspect amoxicillin is the cause of yellowing, consider the duration of the antibiotic course and examine other potential factors like poor oral hygiene or underlying health issues that might impact tooth color.
Here’s what to do: Maintain diligent oral hygiene. Brush and floss twice daily. Regular dental checkups are vital for early detection and treatment of any underlying dental issues. If the discoloration persists after completing the amoxicillin course and maintaining good oral hygiene, consult your dentist to rule out other potential causes such as dental fluorosis or other medical conditions. They can provide a proper diagnosis and recommend appropriate treatment if needed.
Remember: This information isn’t a replacement for professional medical advice. Always consult your doctor or dentist for any concerns regarding medication side effects or dental health issues.
- Amoxicillin Teeth Yellowing: A Comprehensive Guide
- Understanding the Staining Process
- Effective Cleaning Strategies
- Prevention and Minimization
- When to Seek Professional Help
- Understanding Amoxicillin and its Effects on Teeth
- Factors Contributing to Discoloration
- Minimizing the Risk
- The Mechanism Behind Amoxicillin-Induced Tooth Discoloration
- Tetracycline’s Role in Comparison
- Factors Affecting Discoloration
- Treatment Options
- Identifying Amoxicillin-Related Tooth Staining
- Factors Influencing the Severity of Tooth Discoloration
- Drug Formulation and Administration
- Individual Genetic Predisposition
- Oral Hygiene Practices
- Timing of Treatment
- Prevention and Minimizing the Risk of Yellow Teeth
- Dietary Considerations
- Additional Tips
- Protecting Your Enamel
- Treatment Options for Amoxicillin-Related Tooth Staining
- Professional Cleaning and Polishing
- Teeth Whitening
- Microabrasion
- Dental Bonding or Veneers
- Dietary Changes
- Regular Dental Checkups
- Important Note:
Amoxicillin Teeth Yellowing: A Comprehensive Guide
Amoxicillin staining is usually temporary and resolves with proper oral hygiene. Brushing and flossing regularly, ideally after every meal, significantly reduces staining.
Understanding the Staining Process
The yellow discoloration stems from amoxicillin interacting with the enamel’s porous structure. This isn’t a permanent alteration, but rather a surface-level discoloration. The intensity depends on several factors including the dosage, duration of treatment, and individual oral health. Increased plaque build-up exacerbates the issue.
Effective Cleaning Strategies
Professional cleaning by a dentist is highly recommended. They can remove surface stains efficiently. Consider using a soft-bristled toothbrush to avoid enamel abrasion. Rinsing with a fluoride mouthwash can help remineralize teeth. For stubborn stains, your dentist might suggest additional treatments such as polishing.
Prevention and Minimization
Hydration is key; drinking plenty of water helps wash away food particles and amoxicillin residue. Maintain good oral hygiene throughout your treatment. Inform your dentist about the amoxicillin use; they can monitor the situation and provide personalized advice.
When to Seek Professional Help
If staining persists after completing the amoxicillin course and improving oral hygiene, consult your dentist. Persistent discoloration might indicate another underlying issue. They can determine the cause and suggest appropriate solutions.
Understanding Amoxicillin and its Effects on Teeth
Amoxicillin itself doesn’t directly stain teeth yellow. The discoloration you might see is usually linked to a secondary effect – the medication’s impact on oral bacteria. Amoxicillin fights bacterial infections, but this disruption can sometimes lead to an overgrowth of other types of bacteria, potentially increasing the risk of discoloration.
Factors Contributing to Discoloration
Several factors influence whether or not amoxicillin contributes to yellow teeth. Age plays a role: younger children are potentially more susceptible due to their developing teeth. Poor oral hygiene significantly increases this risk. Regular brushing and flossing are crucial for preventing discoloration regardless of medication use. Existing dental conditions may also heighten sensitivity to this effect. Finally, the duration of amoxicillin treatment affects the chance of discoloration. Longer courses increase the risk.
Minimizing the Risk
Maintain diligent oral hygiene throughout your amoxicillin course. Brush twice daily with fluoride toothpaste and floss regularly. Consider using a mouthwash recommended by your dentist. Schedule a dental check-up after completing your amoxicillin treatment to monitor your teeth’s condition. If discoloration occurs, discuss professional teeth whitening options with your dentist.
The Mechanism Behind Amoxicillin-Induced Tooth Discoloration
Amoxicillin doesn’t directly stain teeth. The discoloration arises from its interaction with calcium in developing teeth. Specifically, amoxicillin can interfere with the mineralization process, leading to a disruption in the enamel’s structure.
Tetracycline’s Role in Comparison
Unlike tetracycline antibiotics, which directly bind to calcium in the teeth, amoxicillin’s effect is indirect. Tetracycline stains are often darker and more prevalent. Amoxicillin discoloration typically appears as a yellowish-brown hue, and the severity depends on the dosage and duration of antibiotic treatment, as well as the child’s age (younger children are more susceptible).
Factors Affecting Discoloration
Several factors influence the likelihood and severity of amoxicillin-induced discoloration. These include the child’s age (during tooth development), the dosage and duration of the amoxicillin course, and individual genetic predisposition. Proper dental hygiene practices might not entirely prevent staining but can help minimize its impact.
Treatment Options
Unfortunately, there’s no guaranteed cure for amoxicillin-related tooth discoloration. However, professional whitening treatments, such as microabrasion or bleaching, may lighten the affected areas in some cases. Early detection is key, so regular dental checkups are recommended for children who have taken amoxicillin during tooth development.
Identifying Amoxicillin-Related Tooth Staining
Examine your teeth carefully in natural light. Look for yellow or brownish discoloration, particularly in the grooves and crevices of your teeth. This staining often appears as diffuse discoloration, rather than localized spots.
Pay close attention to the timing. Did the discoloration appear after a course of amoxicillin? A temporal correlation strongly suggests a link. Note the duration of amoxicillin treatment – longer courses might increase the risk of staining.
Consider your age. Young children are more susceptible to amoxicillin-related tooth staining because their teeth are still developing. Adult teeth are less likely to be affected.
Compare your teeth to photos of amoxicillin-induced staining available online. Several dental resources show examples of this discoloration. This can help you gauge the severity and nature of your staining.
Schedule an appointment with your dentist. They can perform a thorough examination and offer a definitive diagnosis. They can also discuss potential treatment options, such as professional cleaning or bleaching.
| Factor | Indication of Amoxicillin-Related Staining |
|---|---|
| Color | Yellow or brownish discoloration |
| Location | Diffuse staining, often in grooves |
| Timing | Appearance after amoxicillin use |
| Age | Higher likelihood in children |
Remember, only a dentist can provide a confirmed diagnosis and recommend the best course of action. Self-diagnosis should not replace professional dental care.
Factors Influencing the Severity of Tooth Discoloration
The intensity of amoxicillin-related tooth discoloration varies significantly. Several key factors contribute to this variation. Age plays a crucial role; younger children, whose teeth are still developing, may experience more noticeable staining than adults. The total dosage of amoxicillin administered directly impacts staining; higher cumulative doses increase the risk of more pronounced discoloration.
Drug Formulation and Administration
The specific formulation of amoxicillin matters. Liquid amoxicillin, due to its prolonged contact with teeth, often leads to more severe staining compared to capsules or tablets. The frequency of administration also influences discoloration; more frequent doses mean more prolonged exposure to the antibiotic.
Individual Genetic Predisposition
Genetic factors influence tooth structure and enamel porosity. Individuals with naturally thinner or more porous enamel may be more susceptible to noticeable discoloration from amoxicillin. This inherent variability contributes to the wide range of staining observed.
Oral Hygiene Practices
Consistent and thorough oral hygiene significantly mitigates discoloration risk. Regular brushing and flossing remove food particles and plaque, minimizing the antibiotic’s interaction time with teeth. This simple practice can help reduce the severity of staining.
Timing of Treatment
The timing of amoxicillin administration during tooth development significantly impacts the final outcome. Treatment during the critical stages of tooth formation may result in more extensive and permanent discoloration. Post-development treatment generally leads to milder effects.
Prevention and Minimizing the Risk of Yellow Teeth
Maintain excellent oral hygiene. Brush twice daily with fluoride toothpaste, for at least two minutes each time, using gentle circular motions. Floss daily to remove plaque and food particles from between your teeth.
Dietary Considerations
- Limit sugary drinks and snacks. Excessive sugar consumption fuels bacterial growth, leading to discoloration.
- Reduce consumption of staining foods and beverages like coffee, tea, red wine, and berries. Rinse your mouth with water after consuming these.
- Increase your intake of water to help naturally cleanse your mouth.
Regular dental checkups are vital. Schedule professional cleanings every six months to remove built-up plaque and tartar, which contribute to staining.
Additional Tips
- Consider using a straw for dark-colored drinks to minimize contact with your teeth.
- Explore professional whitening options with your dentist if you desire whiter teeth. Discuss the various methods available and their potential side effects.
- Quit smoking. Tobacco use significantly stains teeth.
Protecting Your Enamel
Avoid abrasive toothpastes or brushing too vigorously, as this can wear down enamel, making teeth more prone to staining. A soft-bristled toothbrush is recommended.
Treatment Options for Amoxicillin-Related Tooth Staining
Addressing amoxicillin-related tooth discoloration often involves professional dental intervention. Don’t hesitate to schedule an appointment with your dentist for a proper assessment.
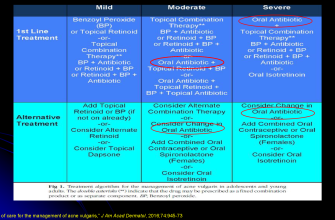
Professional Cleaning and Polishing
Your dentist will likely begin with a professional cleaning to remove surface stains. This typically involves scaling and polishing to gently remove the discoloration. The effectiveness varies depending on the severity and type of staining.
Teeth Whitening
- In-office whitening: Provides faster, more dramatic results than at-home treatments. Your dentist uses a high-concentration bleaching agent for a noticeable improvement in a single visit. However, this is generally more expensive.
- At-home whitening: Offers a more affordable option. Your dentist might provide custom-fitted trays and bleaching gel for you to use at home over several weeks. Consistency is key for optimal results. This method may be less effective for deep stains.
Microabrasion
For more stubborn stains, microabrasion might be recommended. This technique involves carefully removing the stained enamel layer using a mild abrasive paste and a rotating brush. It’s generally more abrasive than polishing, so the dentist will assess if it’s suitable for your teeth.
Dental Bonding or Veneers
In cases of severe or deep staining unresponsive to other treatments, cosmetic procedures like bonding or veneers can mask the discoloration. Bonding involves applying a tooth-colored resin to the stained area, while veneers are thin shells cemented onto the front surface of the teeth. These options are more permanent and costly than other approaches.
Dietary Changes
While not directly addressing the stain, reducing consumption of staining foods and drinks – like coffee, tea, red wine, and berries – can prevent further discoloration and help maintain the improved appearance of your teeth after treatment.
Regular Dental Checkups
- Maintaining good oral hygiene with regular brushing and flossing minimizes the risk of future staining.
- Routine checkups allow your dentist to monitor your teeth and address any concerns early.
Important Note:
The best treatment option depends on the severity of the staining and your individual needs. Consult your dentist to determine the most appropriate course of action for your specific situation.