Yes, amoxicillin can lead to dark stools in some cases. This phenomenon may arise due to various factors linked to the medication’s effects on the gastrointestinal tract or interactions with food and other substances. Understanding the underlying mechanisms can help you manage any concerns related to this side effect.
Amoxicillin is an antibiotic commonly used to treat bacterial infections. While it is generally well-tolerated, some individuals may experience changes in their stool color. Dark stools can indicate the presence of certain substances, such as blood or iron, which may result from amoxicillin’s influence on bacterial flora or the body’s natural response to antibiotic treatment.
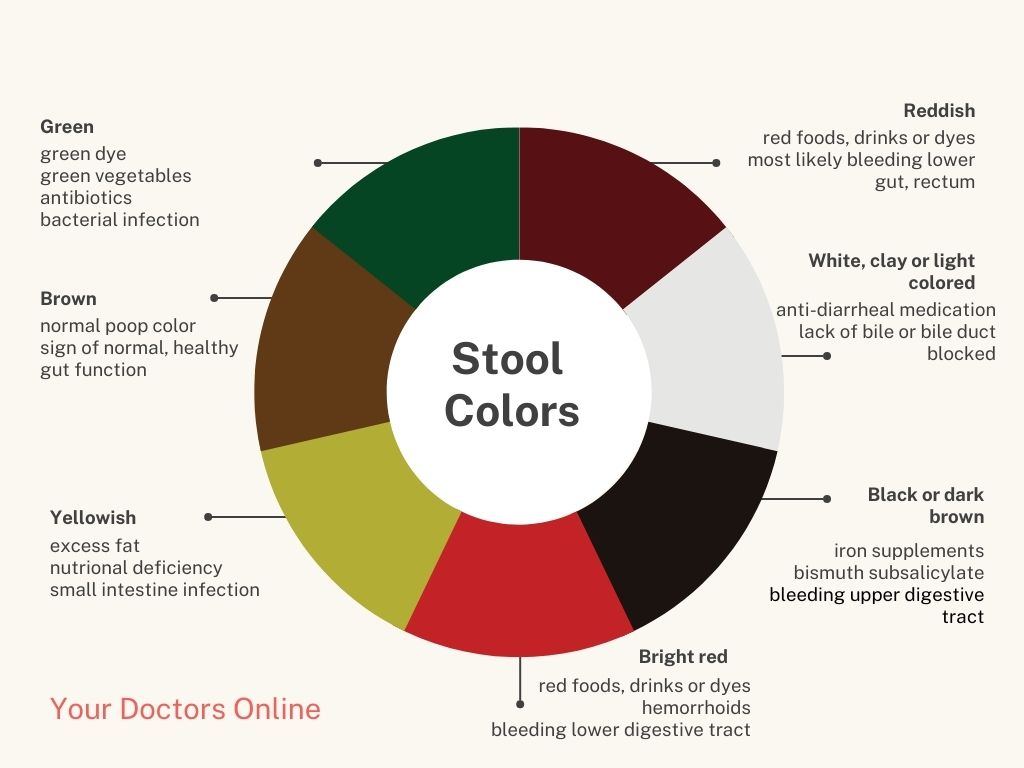
If you notice dark stools while taking amoxicillin, it’s advisable to monitor the situation closely. Assess other symptoms you may experience, such as discomfort or gastrointestinal upset. If dark stools persist or if you observe signs of bleeding, such as red or black tarry stools, seeking medical attention promptly will ensure appropriate evaluation and care.
- Can Amoxicillin Cause Dark Stools?
- Understanding Amoxicillin and Its Uses
- Common Applications of Amoxicillin
- Side Effects and Precautions
- Common Side Effects of Amoxicillin
- Digestive Issues
- Allergic Reactions
- Possible Reasons for Dark Stools While Taking Amoxicillin
- Iron Supplements
- Dietary Factors
- When to Seek Medical Advice for Dark Stools
- Alternatives to Amoxicillin and Their Effects on Stools
- Azithromycin
- Ciprofloxacin
- Doxycycline
- Probiotics
Can Amoxicillin Cause Dark Stools?
Amoxicillin can lead to dark stools in some individuals, primarily due to the antibiotic’s interaction with gut flora. Alterations in digestive bacteria can affect stool color. If you notice dark stools after starting amoxicillin, it’s essential to assess other potential causes, such as dietary changes or the intake of iron supplements, which can also contribute to stool discoloration.
While dark stools aren’t a direct side effect of amoxicillin, they may indicate bleeding in the gastrointestinal tract. This condition requires immediate medical attention. Monitoring your stool color and consistency can help identify potential issues early. If dark stools persist or are accompanied by other concerning symptoms like abdominal pain or blood, consult a healthcare provider promptly.
Individuals taking amoxicillin should maintain an open line of communication with their healthcare providers regarding any unusual side effects. Keep a record of any changes in bowel habits or stool appearance to facilitate discussions during medical appointments.
Understanding Amoxicillin and Its Uses
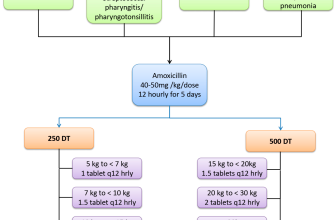
Amoxicillin is a penicillin-type antibiotic used to treat various bacterial infections. It’s frequently prescribed for conditions such as pneumonia, bronchitis, and infections of the ear, nose, throat, and urinary tract. This medication fights bacteria by inhibiting their growth, helping the immune system eliminate the infection effectively.
Common Applications of Amoxicillin
This antibiotic is particularly useful for treating infections caused by specific bacteria, including streptococcus and staphylococcus species. Healthcare professionals often recommend it for pediatric patients with infections like otitis media, as it is generally safe for children. Dosing varies based on age, weight, and the type of infection.
Side Effects and Precautions
While amoxicillin is generally well-tolerated, it can cause side effects in some patients, including gastrointestinal disturbances. Rarely, these disturbances may lead to the appearance of dark stools, which could indicate bleeding in the digestive tract. If you notice this symptom or experience severe side effects, consult your healthcare provider immediately. Always inform your doctor of pre-existing conditions, especially liver or kidney issues, prior to beginning treatment.
Common Side Effects of Amoxicillin
Patients frequently experience mild side effects when taking amoxicillin. Understanding these can help manage expectations and encourage proper usage.
Digestive Issues
- Nausea: Some individuals report feeling queasy after taking amoxicillin. Taking it with food can help alleviate this.
- Diarrhea: This is a common occurrence, as antibiotics can disrupt gut flora. Staying hydrated is essential.
- Vomiting: Less often, patients might experience vomiting. If this occurs, consult a healthcare provider for further guidance.
Allergic Reactions
- Rash: Skin reactions may manifest as rashes. Monitoring for this can prevent complications.
- Itching: Some individuals report itching as a side effect, possibly indicating an allergic response. Contact your doctor if this happens.
- Swelling: Facial or throat swelling may indicate a serious allergic reaction known as angioedema. Immediate medical attention is required in such cases.
While these side effects are common, any severe or persistent symptoms should prompt a discussion with a healthcare professional to ensure safety and effective treatment.
Possible Reasons for Dark Stools While Taking Amoxicillin
Dark stools during amoxicillin treatment can occur due to several factors. First, this antibiotic may upset the balance of gut bacteria, leading to altered digestion and absorption of nutrients. This imbalance can cause changes in stool color.
Iron Supplements
If you’re taking iron supplements alongside amoxicillin, this can also contribute to darker stools. Iron is known for causing a darker appearance, which can combine with antibiotic effects to intensify the change in stool color.
Dietary Factors
Your diet plays a crucial role as well. Foods high in iron, such as red meat or leafy greens, may darken stool color, especially in combination with antibiotic use. Additionally, consuming black licorice or blueberries can also lead to darker stools.
| Factor | Effect on Stool Color |
|---|---|
| Amoxicillin | May alter gut flora |
| Iron Supplements | Can cause darker stools |
| Diet | Foods high in iron or dark pigments |
If dark stools persist or are accompanied by other symptoms like abdominal pain or blood, consult a healthcare provider for further evaluation.
When to Seek Medical Advice for Dark Stools
Consult a healthcare professional if you notice dark stools that persist for more than a couple of days. This could signal gastrointestinal bleeding or other serious conditions. Pay attention to additional symptoms such as abdominal pain, dizziness, or vomiting, especially if the vomit resembles coffee grounds. These signs indicate a need for immediate medical evaluation.
If you have a history of ulcers, liver disease, or blood clotting disorders, reach out to your doctor promptly upon noticing dark stools. Inform them about any medications you’re taking, including over-the-counter products and supplements, as some can cause discoloration.
Monitor any changes in bowel habits. If dark stools accompany ongoing diarrhea or constipation, it’s advisable to seek advice. Discuss lifestyle factors, diet, and any recent illnesses during your consultation to assist in accurate diagnosis and treatment.
Alternatives to Amoxicillin and Their Effects on Stools
Consider alternatives like azithromycin, ciprofloxacin, and doxycycline if amoxicillin isn’t suitable. Each has distinct effects on the gastrointestinal tract.
Azithromycin
Azithromycin is effective against various bacterial infections. It generally does not cause changes in stool color; however, some individuals report mild diarrhea. Ensure adequate hydration while using this antibiotic to mitigate potential gastrointestinal discomfort.
Ciprofloxacin
Ciprofloxacin treats a range of infections and can affect bowel movements. Some users may experience darker stools, often linked to liver function changes during treatment. Monitoring your health and discussing any persistent changes with a healthcare provider is advisable.
Doxycycline
Doxycycline is another alternative that can treat respiratory and skin infections. Like azithromycin, it rarely causes dark stools. However, some people may experience gastrointestinal upset, including nausea, which can indirectly affect stool consistency. Taking doxycycline with food can help reduce irritation.
Probiotics
Incorporating probiotics can help maintain gut health during and after antibiotic treatment. They can counteract antibiotic-related diarrhea and contribute positively to stool consistency without altering its color. Foods like yogurt or supplements may be beneficial.
- Azithromycin: Mild diarrhea, no dark stools.
- Ciprofloxacin: Potential for darker stools, symptomatic monitoring needed.
- Doxycycline: Gastrointestinal upset possible; take with food.
- Probiotics: Support gut health, improve stool consistency.
Communication with your healthcare provider remains essential when considering alternatives to amoxicillin. Make informed decisions based on your specific health needs.