Ciprofloxacin’s effects typically begin within one to two hours of ingestion. You’ll notice the maximum therapeutic concentration within 1-4 hours depending on the dosage form and individual factors. The medication’s effects generally persist for 12-24 hours, although this can vary.
Factors influencing these timings include the specific dosage form (tablet, injection), your metabolism, kidney function, and the presence of other medications. Absorption rates differ between oral and intravenous administration; intravenous administration shows faster onset times.
Remember: This information serves as a general guideline. Always consult your doctor or pharmacist for precise details tailored to your individual circumstances and health profile. They can provide specific information about expected onset, peak concentration, and duration based on your prescription and medical history. Never adjust your dosage or frequency without medical guidance.
- Ciprofloxacin: Onset, Peak, and Duration of Action
- Peak Plasma Concentrations
- Duration of Action and Dosing
- Factors Influencing Pharmacokinetics
- Monitoring Treatment Response
- Understanding Ciprofloxacin’s Onset of Action
- Peak Plasma Concentrations of Ciprofloxacin
- Duration of Ciprofloxacin’s Therapeutic Effect
- Factors Influencing Treatment Duration
- Factors Influencing Ciprofloxacin Pharmacokinetics
- Clinical Implications of Ciprofloxacin’s Pharmacokinetic Profile
- Dosage Adjustments and Patient Populations
- Duration of Therapy and Resistance
Ciprofloxacin: Onset, Peak, and Duration of Action
Ciprofloxacin’s onset of action varies depending on the route of administration and the specific infection being treated. Oral administration typically shows effects within 1-2 hours. Intravenous administration is faster, with effects often seen within 30-60 minutes. Remember these are general timelines, and individual responses can differ.
Peak Plasma Concentrations
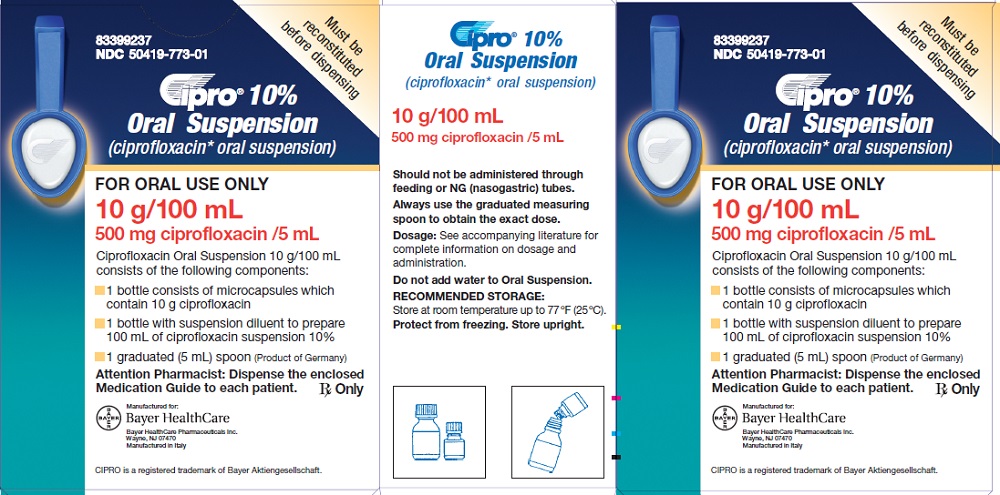
Peak plasma concentrations are achieved approximately 1-4 hours after an oral dose and shortly after intravenous infusion is complete. Specific timing depends on factors like dosage and patient metabolism. These peak levels are critical for achieving sufficient drug concentration at the infection site.
Duration of Action and Dosing
Ciprofloxacin’s duration of action is related to its half-life, generally around 4-7 hours. However, this doesn’t dictate the treatment duration, which is determined by the infection’s severity and response to treatment. A doctor will prescribe a course appropriate for your individual needs. Typical dosing regimens involve twice-daily administration to maintain therapeutic levels throughout the day. Always follow your doctor’s instructions for dosage and frequency.
Factors Influencing Pharmacokinetics
Age, renal function, and hepatic function significantly affect Ciprofloxacin’s pharmacokinetics. Elderly patients and those with impaired kidney or liver function may experience slower elimination, potentially necessitating dosage adjustments. Your physician will consider these factors when determining your treatment plan. Always discuss any pre-existing conditions with your doctor before starting Ciprofloxacin.
Monitoring Treatment Response
Regular monitoring of infection symptoms is crucial. If you don’t see improvement within a few days, contact your healthcare provider. They can assess your progress and adjust treatment accordingly. Don’t stop taking Ciprofloxacin without consulting your doctor, even if you feel better.
Understanding Ciprofloxacin’s Onset of Action
Ciprofloxacin, a fluoroquinolone antibiotic, begins working quickly. You’ll see a reduction in bacterial growth within hours of taking a dose.
However, the noticeable improvement in symptoms depends on several factors:
- Type of infection: A simple urinary tract infection might show improvement sooner than a severe pneumonia.
- Severity of infection: A more severe infection requires more time for the antibiotic to overcome the bacterial load.
- Patient factors: Individual metabolism and overall health influence drug absorption and efficacy.
- Dosage and administration: Following prescribed dosage instructions is critical for optimal results.
While a reduction in bacterial growth happens rapidly, complete symptom resolution takes longer. Don’t expect immediate relief.
- Peak plasma concentrations: Typically occur within 1-4 hours of oral administration, influencing the speed of symptom improvement.
- Duration of therapy: Treatment courses usually last several days, sometimes weeks, depending on the infection.
- Consistent medication: Maintaining a consistent dosing schedule is key. Skipping doses prolongs the infection and may lead to antibiotic resistance.
Always consult your doctor or pharmacist for personalized guidance on expected onset, peak effects, and duration of treatment for your specific situation. They can accurately assess your condition and provide tailored advice.
Peak Plasma Concentrations of Ciprofloxacin
Ciprofloxacin reaches peak plasma concentrations within 1-2 hours of oral administration. This timeframe can vary slightly depending on factors like formulation and individual patient characteristics.
For intravenous administration, peak levels generally occur within 30-60 minutes. However, achieving therapeutic concentrations is influenced by dosage and infusion rate.
Specific peak concentrations are highly variable and depend on numerous factors. A 500 mg oral dose might produce peak levels between 2 and 4 µg/mL, while a 400 mg IV dose may yield higher peaks, potentially exceeding 5 µg/mL. Consult detailed pharmacokinetic data for precise ranges.
Factors influencing peak plasma levels include: Food intake significantly impacts oral absorption, delaying peak time and reducing peak concentrations. Renal function plays a critical role; impaired renal function leads to increased levels and prolonged half-life.
Clinical significance: Monitoring peak concentrations isn’t usually routine for uncomplicated infections. However, in serious infections or with renal impairment, therapeutic drug monitoring may be necessary to optimize dosing and avoid toxicity. A physician should guide these decisions.
Important Note: This information is for educational purposes only and does not constitute medical advice. Always consult with a healthcare professional for any health concerns or before making any decisions related to your health or treatment.
Duration of Ciprofloxacin’s Therapeutic Effect
The duration of Ciprofloxacin’s therapeutic effect varies greatly depending on the infection treated and the patient’s individual factors. Generally, a course of treatment lasts from 7 to 14 days for uncomplicated infections. However, more serious infections, like pneumonia or osteomyelitis, may require significantly longer treatment periods, potentially extending to several weeks or even months under a doctor’s guidance.
Factors Influencing Treatment Duration
Several factors influence how long Ciprofloxacin treatment should continue. These include the specific bacteria causing the infection, its susceptibility to Ciprofloxacin, the severity of the illness, the patient’s immune response, and the location of the infection. For example, a urinary tract infection might clear up within a week, whereas a bone infection requires a more prolonged treatment regimen. Your doctor will determine the appropriate duration based on your specific situation. Regular monitoring and clinical assessment are critical to ensure the infection is resolving and to adjust the treatment accordingly.
Always follow your physician’s prescribed course of Ciprofloxacin, even if you feel better before finishing the medication. Stopping treatment prematurely can lead to treatment failure and potential complications, including the development of antibiotic resistance.
Factors Influencing Ciprofloxacin Pharmacokinetics
Ciprofloxacin absorption varies significantly. Oral bioavailability typically reaches 70-80%, but food reduces absorption, delaying peak plasma concentrations (Cmax) and slightly decreasing the area under the curve (AUC). This means taking Ciprofloxacin on an empty stomach generally optimizes absorption.
Renal function plays a major role. Ciprofloxacin is primarily excreted unchanged via the kidneys. Patients with impaired renal function experience slower elimination, leading to higher and prolonged plasma concentrations. Dose adjustments are necessary based on creatinine clearance to prevent toxicity. Consider using a dosage calculator for accurate adjustments.
Age also impacts pharmacokinetics. Elderly patients often have reduced renal function and decreased hepatic metabolism, resulting in prolonged half-life and increased risk of adverse effects. Therefore, close monitoring and potential dose reduction are often necessary.
Hepatic impairment influences Ciprofloxacin’s metabolism to a lesser extent than renal impairment. However, decreased hepatic clearance can still lead to modestly elevated plasma levels. Monitor patients with liver disease closely.
Drug interactions are a significant concern. Drugs that affect renal function or compete for tubular secretion can alter Ciprofloxacin’s elimination. Examples include probenecid, cimetidine, and some antacids. Consult drug interaction databases before prescribing Ciprofloxacin concurrently with other medications.
Finally, genetic factors can subtly influence Ciprofloxacin metabolism. Although not routinely considered in standard dosing, variations in genes encoding drug transporters and metabolizing enzymes can affect individual responses to the drug. This highlights the importance of close clinical monitoring and responsiveness to patient symptoms.
Clinical Implications of Ciprofloxacin’s Pharmacokinetic Profile
Ciprofloxacin’s rapid absorption, typically reaching peak plasma concentrations within 1-2 hours, dictates its dosing frequency. This rapid onset allows for quicker symptom relief in acute infections, but also necessitates careful consideration of dosing intervals to maintain therapeutic levels. A once-daily regimen might suffice for some infections, while twice-daily dosing is often preferred for more severe or complicated cases. Dosage adjustments are necessary for patients with impaired renal function due to its primarily renal excretion.
Dosage Adjustments and Patient Populations
Patients with renal impairment require reduced doses to prevent toxicity. Creatinine clearance accurately predicts drug elimination. Dosage adjustments based on creatinine clearance are crucial to prevent accumulation and potential adverse effects. Similarly, elderly patients, who often exhibit decreased renal function, necessitate dose modifications. Concomitant medication use may also influence ciprofloxacin pharmacokinetics; consider potential drug interactions, including those affecting renal clearance or metabolism, when prescribing.
Duration of Therapy and Resistance
The duration of ciprofloxacin therapy directly relates to the pharmacokinetic profile and the infection’s severity and response. Shorter treatment courses are preferred to minimize the risk of resistance development. However, inadequate treatment duration can lead to treatment failure and promote resistance, hence the need for careful assessment of individual patient response and adherence to recommended treatment guidelines.