Yes, Amoxicillin is a member of the penicillin antibiotic family, but it is chemically distinct from traditional penicillin. Amoxicillin offers a broader spectrum of activity against bacteria, which makes it effective for treating various infections, including respiratory and urinary tract infections.
When prescribed Amoxicillin, it’s important to be aware of potential allergic reactions, especially if you have a known allergy to penicillin. While many individuals tolerate Amoxicillin without any issues, those with penicillin allergies should consult their healthcare provider to explore suitable alternatives.
For effective treatment, follow the prescribed dosage and duration, as stopping antibiotics prematurely may lead to a resurgence of the infection. Always communicate openly with your healthcare provider regarding any side effects or concerns you may experience during your course of treatment.
- Understanding Amoxicillin and Its Relation to Penicillin
- Allergies and Cross-Reactivity
- Indications and Usage
- Amoxicillin: Composition and Mechanism of Action
- The Role of Penicillin in Amoxicillin’s Effectiveness
- Mechanism of Action
- Comparative Benefits
- Comparing Amoxicillin and Other Penicillin Derivatives
- Amoxicillin vs. Penicillin G
- Amoxicillin vs. Dicloxacillin
- Clinical Implications of Amoxicillin in Penicillin-Allergic Patients
Understanding Amoxicillin and Its Relation to Penicillin
Amoxicillin is a member of the penicillin family, classified as a broad-spectrum antibiotic. It contains a beta-lactam ring, which is characteristic of penicillin antibiotics, aiding in its ability to combat bacterial infections. This structural component allows amoxicillin to inhibit bacterial cell wall synthesis, leading to cell lysis and death. It effectively treats respiratory infections, urinary tract infections, and skin infections, among others.
Allergies and Cross-Reactivity
Patients with a known allergy to penicillin should approach amoxicillin with caution. About 10% of individuals allergic to penicillin may also react to amoxicillin due to their structural similarities. Consulting a healthcare professional before taking amoxicillin, particularly for those with penicillin allergies, is crucial to avoid adverse reactions.
Indications and Usage
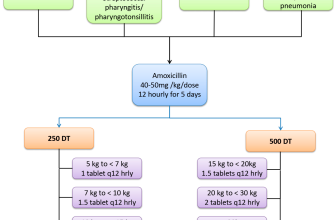
Amoxicillin is commonly prescribed for both adults and children. It is often used in combination with other medications to treat more complex infections. This antibiotic is typically administered orally and comes in various forms, including tablets and liquid suspension. Adhering to the prescribed dosage duration is vital for ensuring complete eradication of the infection and minimizing the risk of resistance development.
Amoxicillin: Composition and Mechanism of Action
Amoxicillin consists of a modified penicillin scaffold, which enhances its antibacterial properties. This semisynthetic antibiotic includes a beta-lactam ring, a core structure that allows it to interfere with bacterial cell wall synthesis. The addition of an amino group differentiates amoxicillin from other penicillins, increasing its effectiveness against a broader spectrum of gram-positive and certain gram-negative bacteria.
The mechanism of action of amoxicillin involves binding to penicillin-binding proteins (PBPs) present in bacterial cell membranes. By inhibiting these proteins, amoxicillin disrupts peptidoglycan cross-linking, crucial for maintaining the structural integrity of the bacterial cell wall. The result of this disruption is bacterial lysis and cell death, making amoxicillin an effective treatment for various infections.
Amoxicillin is commonly prescribed for respiratory tract infections, urinary tract infections, and skin infections. Its wide application stems from its comparative safety, ease of use, and ability to combat resistant bacterial strains, as it is often paired with clavulanic acid to counteract beta-lactamase-producing bacteria.
Consider dosage and potential interactions when administering amoxicillin. Standard adult prescriptions typically range from 500 mg to 875 mg every eight to twelve hours, depending on the severity of the infection. Adjustments are necessary for patients with renal impairment to prevent accumulation and toxicity.
Patient adherence to the prescribed course plays a significant role in treatment success. Educating patients about the importance of completing their prescription, even if symptoms improve, ensures effective eradication of the infection and minimizes resistance development.
The Role of Penicillin in Amoxicillin’s Effectiveness
Amoxicillin combines penicillin with a modified structure that enhances its ability to combat infections. This modification allows it to withstand certain bacterial defenses, making it a powerful antibiotic. Understanding how penicillin contributes to this process is key to grasping why amoxicillin is widely used in treating bacterial infections.
Mechanism of Action
Penicillin functions by inhibiting bacterial cell wall synthesis. This action is crucial because it leads to cell lysis and ultimately bacterial death. Amoxicillin maintains this core mechanism, allowing it to target a broader range of bacteria, including some that are resistant to other penicillin derivatives. The addition of a hydroxyl group in amoxicillin increases its cell permeability and stability, making it more effective against various strains.
Comparative Benefits
Amoxicillin demonstrates effectiveness against both gram-positive and some gram-negative bacteria, expanding treatment options. Its capacity to resist breakdown by certain beta-lactamases enhances its therapeutic range. Additionally, when paired with potassium clavulanate, it becomes vital in combating resistant bacterial strains, as this combination inhibits beta-lactamase enzymes that would otherwise degrade the drug.
| Bacteria Type | Amoxicillin Action |
|---|---|
| Gram-positive | Effective against Staphylococcus and Streptococcus |
| Gram-negative | Effective against E. coli and Haemophilus influenzae |
| Beta-lactamase producers | Can be combined with clavulanate to enhance effectiveness |
Incorporating penicillin’s properties into amoxicillin greatly optimizes its antimicrobial activity. This synergy allows healthcare professionals to tackle a wide array of infections, ensuring comprehensive treatment options for patients.
Comparing Amoxicillin and Other Penicillin Derivatives
Amoxicillin combines the benefits of penicillin derivatives with a broader spectrum of activity against various bacteria. Its unique chemical structure enhances absorption and efficacy. Below, we highlight the differences and similarities between Amoxicillin and other common penicillin derivatives.
Amoxicillin vs. Penicillin G
- Amoxicillin has a broader spectrum, effectively treating infections caused by both Gram-positive and Gram-negative bacteria.
- Penicillin G primarily targets Gram-positive bacteria and certain Gram-negative organisms, but not as effectively as Amoxicillin.
- Administration methods vary: Amoxicillin is typically given orally, making it more convenient, while Penicillin G is often administered intravenously for serious infections.
Amoxicillin vs. Dicloxacillin
- Both antibiotics target staphylococci, but Amoxicillin is more versatile in treating other infections.
- Dicloxacillin is specifically effective against penicillin-resistant staphylococci, making it a go-to choice for resistant strains.
- Amoxicillin offers ease of use with its oral formulation, whereas Dicloxacillin may require monitoring during intravenous administration.
When selecting between Amoxicillin and its derivatives, consider the type of infection and resistance patterns. Amoxicillin remains a reliable choice for a wide range of bacterial infections, while other penicillin derivatives might be more suitable depending on resistance or specific bacterial strains.
Clinical Implications of Amoxicillin in Penicillin-Allergic Patients
Patients with a confirmed penicillin allergy should avoid amoxicillin due to its structural similarity to penicillin. It contains a beta-lactam ring, which can trigger allergic reactions in susceptible individuals. The risk of cross-reactivity varies, but studies suggest it may range from 1% to 10% for those with a history of penicillin allergy.
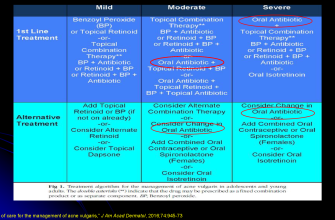
Alternative antibiotics, such as macrolides or cephalosporins, can be considered for treating infections in these patients. Clinicians must assess the severity and type of the allergic reaction when evaluating alternatives. For instance, patients with a history of anaphylaxis should avoid amoxicillin entirely.
Skin testing can help identify true penicillin allergies. Negative test results may allow for a safe trial of amoxicillin under controlled conditions. This practice is increasingly recommended, particularly in non-severe allergy cases, to expand treatment options.
It’s important to document any penicillin allergy in patient records accurately. Mislabeling may lead to unnecessary use of broader-spectrum antibiotics, contributing to resistance issues. Educating patients about their allergies also plays a crucial role in their safety and helps inform healthcare providers during future treatments.
For patients requiring amoxicillin, desensitization protocols exist but should only be conducted in a controlled environment, such as a hospital. This approach involves gradual exposure under medical supervision, suitable for patients with confirmed allergies needing urgent treatment.
Overall, managing penicillin allergy effectively requires thorough assessment, patient education, and consideration of alternative therapies, ensuring safety without compromising treatment efficacy.