Tetracycline’s use against staph infections requires careful consideration. It’s effective against some Staphylococcus aureus strains, but resistance is a significant factor. Always consult a healthcare professional for accurate diagnosis and treatment guidance. Self-treating can be dangerous.
Staphylococcus aureus exhibits varying susceptibility to tetracycline. Methicillin-resistant S. aureus (MRSA), a prevalent concern, often shows resistance. Therefore, determining the specific staph strain and its antibiotic susceptibility profile is paramount before treatment. Laboratory testing provides this crucial information.
If tetracycline is deemed appropriate, the prescribed dosage and duration must be followed precisely. Incomplete treatment regimens can lead to the development of resistant bacteria, further complicating future infections. Pay close attention to any potential side effects and report them immediately to your doctor. These can range from mild gastrointestinal upset to more serious reactions.
Remember: Tetracycline is not a universal solution for staph infections. Alternative antibiotics may be more suitable depending on the infection’s severity and the bacterial strain. Always prioritize expert medical advice over online information or self-medication. Prompt professional guidance is vital for successful treatment and preventing complications.
- Tetracycline for Staph: A Detailed Overview
- Understanding Staph Infections and Their Severity
- Factors Influencing Infection Severity
- Recognizing Serious Staph Infections
- Tetracycline’s Mechanism of Action Against Staph Bacteria
- Ribosomal Binding and Inhibition
- Consequences of Inhibition
- Resistance Mechanisms
- Effectiveness of Tetracycline Against Different Staph Strains
- Potential Side Effects and Risks of Tetracycline Treatment
- Photosensitivity
- Other Potential Side Effects
- When to Seek Medical Attention and Alternative Treatment Options
Tetracycline for Staph: A Detailed Overview
Tetracycline is not always the first-choice antibiotic for Staph infections, especially Staphylococcus aureus, due to widespread resistance. However, it can be effective against some strains. Use only under doctor’s supervision.
Successful treatment hinges on accurate identification of the bacterial strain and its susceptibility to tetracycline. A culture and sensitivity test is critical to guide treatment decisions. This test determines which antibiotics will work best against the specific strain infecting the patient.
Tetracycline’s mechanism involves inhibiting bacterial protein synthesis, thus halting bacterial growth. This action, however, is often compromised by resistance mechanisms in Staphylococcus species, making successful treatment less likely than with other antibiotics.
Common side effects include gastrointestinal upset (nausea, vomiting, diarrhea), photosensitivity (sunburn), and discoloration of teeth in children. These effects vary in severity. Rare but serious side effects exist, demanding immediate medical attention.
| Side Effect | Frequency | Severity |
|---|---|---|
| Nausea | Common | Mild to Moderate |
| Diarrhea | Common | Mild to Moderate |
| Photosensitivity | Common | Mild to Severe |
| Tooth Discoloration (children) | Possible | Moderate |
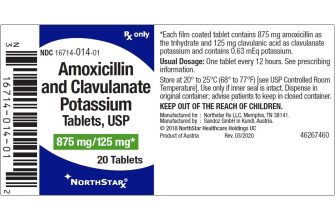
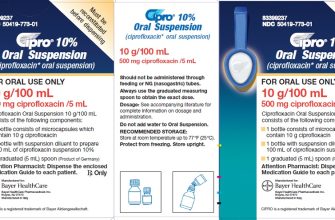
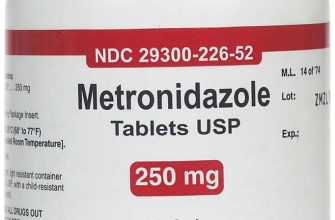
Alternative antibiotics, such as fluoroquinolones, cephalosporins, or glycopeptides, might offer better efficacy against resistant Staph strains. Your doctor will consider the specific infection, the patient’s medical history, and the results of the susceptibility test before prescribing the best course of treatment. Always follow your doctor’s instructions carefully.
Understanding Staph Infections and Their Severity
Staphylococcus aureus, or staph, bacteria reside on skin and in noses harmlessly for many. However, they can cause infections ranging from minor skin irritations to life-threatening conditions. The severity depends on several factors.
Factors Influencing Infection Severity
Location of infection: A skin infection like a boil is typically less serious than pneumonia or bloodstream infection (bacteremia), which can spread rapidly and cause sepsis. Sepsis requires immediate medical attention.
Patient’s immune system: Individuals with weakened immune systems, such as those with HIV, cancer, or diabetes, are at higher risk of severe complications. Their bodies may struggle to fight off the infection.
Type of staph: Methicillin-resistant Staphylococcus aureus (MRSA) is a particularly dangerous strain, resistant to many common antibiotics. Infections with MRSA often require stronger treatment and pose a greater threat.
Prompt medical care: Early diagnosis and treatment are key. Delaying treatment increases the risk of serious complications and spread. See a doctor if you suspect a staph infection.
Recognizing Serious Staph Infections
Signs of severe infection: Seek immediate medical help if you experience high fever, chills, rapid heartbeat, low blood pressure, confusion, or severe pain near the infection site. These symptoms suggest the infection may have spread beyond the initial location.
Antibiotic resistance: Antibiotic resistance is a growing concern, making some infections difficult to treat. Your doctor will determine the best course of action based on the specific type of staph and your overall health.
Tetracycline’s Mechanism of Action Against Staph Bacteria
Tetracycline targets bacterial protein synthesis, specifically inhibiting the binding of aminoacyl-tRNA to the bacterial ribosome’s A-site. This prevents the addition of amino acids to the growing polypeptide chain, halting protein production.
Ribosomal Binding and Inhibition
The drug’s structure allows it to bind reversibly to the 30S ribosomal subunit of Staphylococcus bacteria. This binding directly interferes with the ribosomal function, blocking the attachment of aminoacyl-tRNA molecules. This blockage is crucial because it disrupts the peptide bond formation, a fundamental step in bacterial protein synthesis.
Consequences of Inhibition
The resulting lack of functional proteins leads to bacterial cell death. Staphylococcus aureus, for instance, relies heavily on protein synthesis for survival and replication. Tetracycline’s interruption of this process effectively prevents bacterial growth and multiplication. Note that tetracycline’s broad-spectrum activity means it affects other bacteria besides Staphylococcus, but its effectiveness against specific strains varies. Proper diagnostic testing to confirm Staphylococcus infection and tetracycline susceptibility is always recommended.
Resistance Mechanisms
Bacterial resistance mechanisms against tetracycline can include reduced drug uptake, efflux pump activity that expels the tetracycline from the cell, and ribosomal protection. These mechanisms can diminish the efficacy of tetracycline. Understanding these mechanisms is crucial for clinical management.
Effectiveness of Tetracycline Against Different Staph Strains
Tetracycline’s success against Staphylococcus depends heavily on the specific strain. Resistance is a significant concern.
- S. aureus (Methicillin-Susceptible S. aureus or MSSA): Tetracycline often demonstrates good activity against MSSA. However, increasing resistance necessitates susceptibility testing before treatment.
- S. aureus (Methicillin-Resistant S. aureus or MRSA): MRSA frequently exhibits resistance to tetracycline. Alternative antibiotics are typically preferred.
- Coagulase-Negative Staphylococci (CoNS): Tetracycline’s efficacy varies considerably among CoNS species. Some strains are susceptible, while others demonstrate resistance.
Factors influencing treatment outcomes include:
- Antibiotic concentration: Achieving sufficient drug levels at the infection site is crucial for success.
- Duration of treatment: A shorter course may lead to treatment failure and the development of resistance. Consult guidelines for appropriate treatment duration.
- Patient-specific factors: Kidney or liver function can impact drug metabolism and efficacy.
Always conduct susceptibility testing to guide treatment decisions. Never rely solely on prior experience or general guidelines. This ensures optimal patient outcomes and minimizes the risk of resistance development. Rely on current clinical guidelines and laboratory results.
Potential Side Effects and Risks of Tetracycline Treatment
Tetracycline, while effective against some Staphylococcus infections, carries potential side effects. Gastrointestinal upset, including nausea, diarrhea, and vomiting, is common. This often improves with continued treatment or by taking the medication with food, but inform your doctor if symptoms are severe or persistent.
Photosensitivity
Tetracycline increases skin sensitivity to sunlight. Sunburns are more likely, even with brief sun exposure. Use sunscreen with a high SPF (at least 30) and protective clothing when outdoors during tetracycline treatment. Avoid tanning beds.
Other Potential Side Effects
Less frequent, but still possible side effects include yeast infections, tooth discoloration (primarily in children under 8), and liver problems. Rarely, tetracycline can cause allergic reactions ranging from mild skin rashes to serious anaphylaxis. Severe allergic reactions require immediate medical attention.
Tetracycline can interact with other medications, including antacids, certain antibiotics, and oral contraceptives. Always inform your doctor and pharmacist of all medications you are taking, including over-the-counter drugs and supplements. Pregnancy and breastfeeding may also influence the choice of antibiotics; discuss your circumstances with your doctor.
If you experience any unusual or concerning symptoms during tetracycline treatment, contact your doctor immediately. Early intervention can help manage side effects and prevent complications.
When to Seek Medical Attention and Alternative Treatment Options
Seek immediate medical attention if you experience severe symptoms like high fever (over 101°F or 38.3°C), difficulty breathing, rapid heartbeat, or spreading skin infection. These may indicate a serious complication requiring hospitalization and intravenous antibiotics.
If your staph infection doesn’t improve after 48-72 hours of tetracycline treatment, contact your doctor. They may adjust the medication, prescribe a different antibiotic, or order further testing to identify the specific strain of bacteria and its antibiotic susceptibility.
Alternative treatments focus on supporting your body’s natural healing processes. Proper wound care, including regular cleaning with antiseptic solutions and keeping the area covered with a clean bandage, is paramount. Maintaining good hygiene, including frequent handwashing, helps prevent the spread of infection.
In some cases, your doctor may recommend drainage of an abscess or other surgical interventions to remove infected material. This promotes faster healing and reduces the risk of recurrence. Remember that surgery may be necessary alongside, not instead of, antibiotic treatment.
For mild staph infections responding well to tetracycline, consider incorporating a healthy diet rich in fruits, vegetables, and lean protein to boost your immune system. Sufficient rest is also critical for recovery.
Always consult your physician before starting any new treatment or making changes to your existing regimen. Self-treating can be dangerous and may delay appropriate care, leading to more severe complications. Your doctor will assess your individual needs and recommend the most suitable approach.