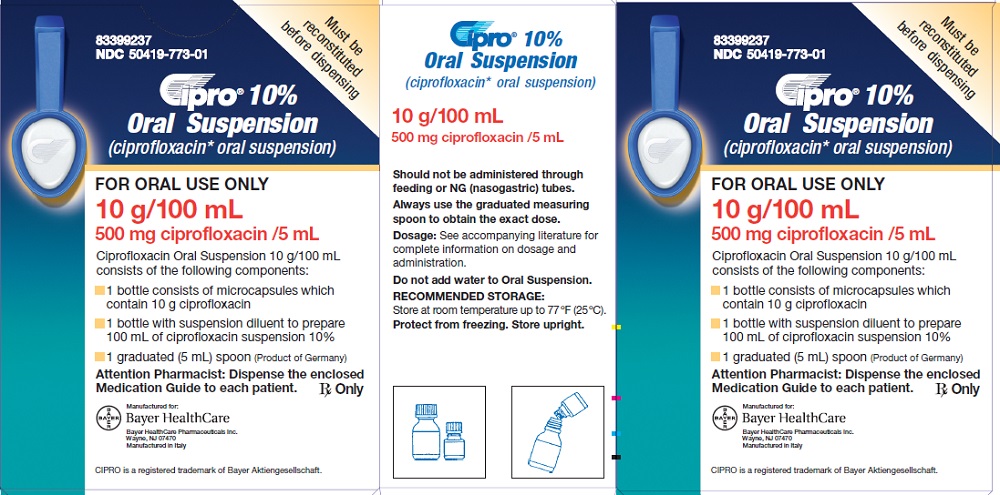
For Pseudomonas aeruginosa infections, Ciprofloxacin dosages vary significantly depending on the infection site and severity. Typical adult intravenous doses range from 400mg every 8-12 hours to a maximum of 1200mg daily. Oral administration usually involves 500mg or 750mg twice daily, but always follow your doctor’s specific prescription. Remember that treatment duration also varies substantially.
Severe or complicated infections, such as those involving the bloodstream (bacteremia) or pneumonia, often require higher doses and prolonged treatment. Your physician will consider factors like your kidney function, age, and the specific strain of Pseudomonas when determining the appropriate dose and duration.
Always consult your doctor or pharmacist. This information is for educational purposes only and should not substitute for professional medical advice. Never adjust your Ciprofloxacin dosage without consulting a healthcare provider. They will carefully assess your individual needs and provide a tailored treatment plan.
Consider potential drug interactions. Ciprofloxacin can interact with other medications. Providing your doctor with a complete list of your current medications is crucial for safe and effective treatment. This proactive approach minimizes the risk of adverse effects and ensures optimal therapeutic outcomes.
- Ciprofloxacin Dosage for Pseudomonas Infections: A Detailed Guide
- Understanding Pseudomonas aeruginosa Infections
- Risk Factors and Symptoms
- Diagnosis and Treatment
- Prevention
- Ciprofloxacin’s Mechanism of Action Against Pseudomonas
- DNA Gyrase Inhibition
- Topoisomerase IV Inhibition
- Clinical Implications
- Standard Ciprofloxacin Dosage Regimens for Pseudomonas
- Adjusting Ciprofloxacin Dosage Based on Patient Factors
- Renal Function
- Age
- Hepatic Function
- Weight
- Concurrent Medications
- Other Considerations
- Common Side Effects and Precautions with Ciprofloxacin
- Treatment Duration and Monitoring for Pseudomonas Infections
- Alternative Treatment Options if Ciprofloxacin Fails
Ciprofloxacin Dosage for Pseudomonas Infections: A Detailed Guide
Treatment of Pseudomonas infections with ciprofloxacin requires careful consideration of the specific infection site and the patient’s clinical status. Dosage varies significantly.
For uncomplicated urinary tract infections (UTIs), typical adult dosage is 250-750 mg twice daily for 7-14 days. More severe UTIs or those involving pyelonephritis may require higher doses and longer treatment durations, potentially up to 400 mg twice daily. Always consult current guidelines for the most up-to-date recommendations.
In cases of lower respiratory tract infections, such as pneumonia, a dosage of 400-750 mg twice daily is usually prescribed. The treatment length depends on the severity, generally ranging from 7 to 21 days.
Skin and soft tissue infections necessitate a dosage ranging from 400 mg to 750 mg twice daily, again with treatment duration determined by individual circumstances and response to therapy. Treatment can last from 7 to 28 days.
Dosage adjustments are frequently needed for patients with impaired renal function. Reduce the dose or extend the dosing interval based on creatinine clearance. Refer to pharmacokinetic data for precise adjustments.
Important Note: Ciprofloxacin is not always the first-line treatment for Pseudomonas infections. Many Pseudomonas strains exhibit resistance to ciprofloxacin. Your physician will determine the appropriate antibiotic based on culture and sensitivity testing results. This information is for educational purposes only and does not replace professional medical advice.
| Infection Site | Typical Dosage (Adults) | Treatment Duration (Days) |
|---|---|---|
| Uncomplicated UTI | 250-750 mg twice daily | 7-14 |
| Complicated UTI/Pyelonephritis | Up to 400 mg twice daily | Variable |
| Lower Respiratory Tract Infection | 400-750 mg twice daily | 7-21 |
| Skin and Soft Tissue Infection | 400-750 mg twice daily | 7-28 |
Always consult a healthcare professional before starting or altering any medication regimen.
Understanding Pseudomonas aeruginosa Infections
Pseudomonas aeruginosa is a common opportunistic pathogen, meaning it usually infects people with weakened immune systems. This bacterium thrives in moist environments, like hospitals and healthcare facilities, making healthcare-associated infections frequent.
Risk Factors and Symptoms
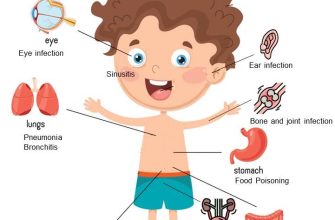
Individuals at higher risk include those with cystic fibrosis, burns, or weakened immune systems due to conditions like HIV or cancer treatment. Symptoms vary widely depending on the infection site. Respiratory infections can present with coughing, shortness of breath, and fever. Urinary tract infections may cause painful urination and frequent urges. Wound infections manifest as pus, pain, swelling, and redness. Sepsis, a life-threatening bloodstream infection, is a serious complication.
Diagnosis and Treatment
Diagnosis typically involves culturing the bacteria from infected samples. Treatment requires antibiotics; however, Pseudomonas aeruginosa is known for its antibiotic resistance. Ciprofloxacin (Cipro) may be used, but resistance is increasing. Combination therapy, often involving aminoglycosides or beta-lactams alongside Cipro, is frequently necessary. The specific antibiotic regimen should always be determined by a doctor based on the infection’s severity and the bacterium’s susceptibility profile.
Prevention
Strict adherence to infection control measures in healthcare settings is crucial. This includes proper hand hygiene, careful sterilization of equipment, and prompt isolation of infected patients. For individuals with chronic conditions increasing their susceptibility, proactive measures to maintain a robust immune system are important. This can include proper nutrition, adequate hydration, and stress management.
Ciprofloxacin’s Mechanism of Action Against Pseudomonas
Ciprofloxacin targets Pseudomonas bacteria by inhibiting DNA gyrase and topoisomerase IV. These enzymes are crucial for bacterial DNA replication, transcription, and repair.
DNA Gyrase Inhibition
DNA gyrase, a type II topoisomerase, introduces negative supercoils into bacterial DNA, relieving torsional strain during replication. Ciprofloxacin binds to the enzyme’s active site, preventing this supercoiling. This blockage halts DNA replication and consequently bacterial growth.
Topoisomerase IV Inhibition
Pseudomonas also relies on topoisomerase IV for DNA segregation during cell division. Ciprofloxacin’s interaction with topoisomerase IV similarly inhibits its function, preventing chromosome separation and ultimately leading to bacterial cell death. The precise contribution of each enzyme to Ciprofloxacin’s overall effect varies depending on the specific Pseudomonas species and the drug concentration.
Clinical Implications
Understanding this dual mechanism of action is key to effective treatment. Resistance mechanisms in Pseudomonas often involve mutations in the gyrA and parC genes, encoding subunits of DNA gyrase and topoisomerase IV, respectively. These mutations alter the drug binding site, reducing Ciprofloxacin’s effectiveness. Monitoring for resistance is, therefore, paramount for successful therapy.
Standard Ciprofloxacin Dosage Regimens for Pseudomonas
Ciprofloxacin treatment for Pseudomonas infections requires careful consideration of the specific infection site and patient factors. Dosage adjustments are often necessary. Always consult current guidelines and local antibiograms for optimal therapy.
Here are some common regimens:
- Uncomplicated Urinary Tract Infections (UTIs): 750 mg twice daily for 7-14 days. Adjust duration based on clinical response.
- Complicated UTIs/Pyelonephritis: 750 mg twice daily, potentially extended to 14-21 days. Consider combination therapy with another antibiotic, guided by antibiogram results and patient factors.
- Lower Respiratory Tract Infections (Pneumonia): 750 mg twice daily or 400 mg twice daily (based on renal function), often for 14 days or longer, often in conjunction with another antibiotic. Length of treatment depends on severity and clinical response.
- Skin and Soft Tissue Infections: 750 mg twice daily for 7-14 days, duration adjusted based on clinical improvement. Combination therapy may be required in severe cases.
- Sepsis: 750-1000 mg every 12 hours or 400 mg every 12 hours (dose-adjusted for renal function). Duration and combination therapy are determined by the severity of illness and the patient’s clinical response. This often involves prolonged treatment.
Important Considerations:
- Renal Function: Dosage adjustments are needed for patients with impaired renal function. Consult prescribing information or use a renal dosing calculator for accurate adjustments.
- Age: Dose adjustments may be necessary for elderly patients due to decreased renal clearance.
- Drug Interactions: Ciprofloxacin interacts with many medications. Always review potential interactions before prescribing.
- Allergy: Assess for prior allergic reactions to fluoroquinolones.
- Monitoring: Close monitoring of the patient’s response to therapy is crucial. Regular clinical assessment, culture, and potentially serum drug level monitoring may be indicated for serious infections.
Disclaimer: This information is for educational purposes only and should not be considered medical advice. Always consult a healthcare professional for diagnosis and treatment of infections.
Adjusting Ciprofloxacin Dosage Based on Patient Factors
Ciprofloxacin dosing for Pseudomonas aeruginosa infections requires careful consideration of several patient-specific factors. Accurate dosage ensures optimal treatment and minimizes adverse effects.
Renal Function
Reduce the Ciprofloxacin dose for patients with impaired renal function. Use a creatinine clearance (CrCl) calculation to guide dosage adjustments. For example, consider halving the dose if CrCl is below 30 mL/min/1.73m². Consult relevant guidelines or clinical pharmacology resources for precise adjustments based on CrCl values. Always refer to the specific product labeling for detailed instructions.
Age
Dosage modification may be necessary for elderly patients (over 65 years) due to decreased renal clearance. Geriatric patients often exhibit reduced drug metabolism and excretion. Carefully monitor these individuals for any adverse reactions. Consider starting with a lower dose and closely monitoring their response.
Hepatic Function
While primarily excreted renally, Ciprofloxacin metabolism involves the liver. Severe hepatic impairment may warrant dose reduction. Consult clinical guidelines for dosage adjustment recommendations in patients with liver dysfunction. Closely monitor for signs of liver toxicity.
Weight
For pediatric patients, Ciprofloxacin dosage is usually calculated based on weight (mg/kg). Refer to age-appropriate dosing charts for recommended dosages. Always monitor the child closely for potential adverse effects.
Concurrent Medications
Several medications can interact with Ciprofloxacin, potentially affecting its metabolism or efficacy. Examples include theophylline, warfarin, and some antacids. Always review a patient’s complete medication list and adjust the Ciprofloxacin dose or consider alternative antibiotics if necessary, based on potential drug interactions.
Other Considerations
- Infection Severity: More severe infections may necessitate higher doses or longer treatment duration.
- Patient Response: Monitor for clinical improvement and adjust the dose or treatment plan accordingly.
- Specific Strain of Pseudomonas: Antibiotic susceptibility testing is crucial to guide therapy. Ciprofloxacin resistance is a growing concern, and treatment should be guided by culture and sensitivity results.
Always consult updated clinical practice guidelines and product labeling for the most current recommendations. Close monitoring of the patient is essential for safe and effective Ciprofloxacin therapy.
Common Side Effects and Precautions with Ciprofloxacin
Ciprofloxacin, while effective against Pseudomonas, can cause side effects. Common gastrointestinal issues include nausea, diarrhea, and abdominal pain. These usually resolve without intervention, but persistent or severe diarrhea warrants immediate medical attention, as it could indicate Clostridium difficile infection.
You might also experience headaches, dizziness, or insomnia. Less frequent but serious side effects include tendon rupture (particularly in older adults or those taking corticosteroids), peripheral neuropathy (numbness or tingling in the extremities), and allergic reactions, ranging from rash to life-threatening anaphylaxis. Report any unusual symptoms promptly to your doctor.
Before starting Ciprofloxacin, inform your doctor about any pre-existing conditions, particularly kidney or liver problems, seizures, or a history of tendon problems. Pregnancy and breastfeeding should also be discussed, as Ciprofloxacin can pass into breast milk. Avoid sun exposure, as photosensitivity is a possible side effect. Finally, understand that Ciprofloxacin interacts with certain medications; your doctor needs a complete medication history to minimize adverse effects.
Remember to follow your prescribed dosage and duration precisely. Do not stop treatment early, even if you feel better, to ensure complete eradication of the infection. This medication should only be used as directed by a healthcare professional.
Treatment Duration and Monitoring for Pseudomonas Infections
Treatment typically lasts 10-14 days, but adjustments depend on the patient’s response and the infection site. Severe or complicated infections may require longer courses, potentially up to several weeks. Always follow your doctor’s specific instructions.
Monitoring is critical. Regular blood tests track drug levels and kidney function. Clinicians assess the infection site for signs of improvement, such as reduced inflammation and drainage. Clinical cultures guide adjustments to the antibiotic regimen, ensuring optimal efficacy. Early detection of treatment failure through close monitoring prevents complications and improves outcomes.
Ciprofloxacin resistance is increasing; therefore, susceptibility testing is essential before initiating treatment. Alternative antibiotics are crucial if resistance is observed. Your doctor will use the results to determine the most appropriate treatment strategy. Regular follow-up appointments are necessary to evaluate progress and make timely adjustments as needed.
Careful monitoring allows for timely intervention should complications arise. Symptoms like worsening pain, fever, or increased discharge require immediate medical attention. This proactive approach significantly improves the chance of a successful treatment outcome.
Alternative Treatment Options if Ciprofloxacin Fails
If Ciprofloxacin treatment proves ineffective against Pseudomonas, your doctor will likely switch to a different antibiotic. Common alternatives include Piperacillin/Tazobactam, Ceftazidime, Cefepime, or Imipenem/Cilastatin. The choice depends on several factors, including the specific Pseudomonas species, its antibiotic susceptibility profile, and your overall health.
Piperacillin/Tazobactam is a broad-spectrum antibiotic frequently used for serious infections. Ceftazidime and Cefepime are cephalosporins effective against many Pseudomonas strains. Imipenem/Cilastatin is a carbapenem, a powerful class of antibiotics reserved for severe infections resistant to other options. A culture and sensitivity test guides antibiotic selection to ensure the best chance of success.
Remember: Antibiotic selection requires careful consideration. Your doctor will conduct further tests to identify the most appropriate alternative. This might involve additional cultures to determine antibiotic resistance patterns or evaluating other contributing factors to your infection.
Aminoglycosides such as Amikacin or Gentamicin may be combined with other antibiotics to enhance efficacy. However, these carry the risk of kidney damage, so close monitoring is necessary.
Always discuss treatment options thoroughly with your physician. They will tailor your treatment plan to your individual needs and circumstances.