Don’t mix amoxicillin and penicillin simultaneously. While both are antibiotics targeting similar bacterial infections, combining them offers no additional benefit and might increase the risk of side effects. Your doctor should always determine the appropriate antibiotic and dosage.
Amoxicillin and penicillin belong to the same class of antibiotics (penicillins), meaning they share a similar mechanism of action. Taking both together won’t make the infection clear faster; instead, it increases the potential for adverse reactions such as digestive upset, allergic reactions, or interactions with other medications. Always follow your doctor’s prescribed regimen strictly.
If you’re prescribed one antibiotic and are concerned about another, discuss this with your healthcare provider before taking any action. They can assess your specific needs and determine the best course of treatment. Remember, proper antibiotic use is crucial for effective treatment and preventing antibiotic resistance.
Seek immediate medical attention if you experience symptoms such as severe allergic reactions (e.g., difficulty breathing, swelling, hives) after taking either amoxicillin or penicillin. Accurate diagnosis and appropriate treatment are vital to your health.
- Mixing Amoxicillin and Penicillin: A Detailed Guide
- Are Amoxicillin and Penicillin the Same?
- Understanding the Chemical Structures of Amoxicillin and Penicillin
- Amoxicillin’s Structure
- Penicillin G’s Structure
- Similar but Different: Mechanisms of Action
- Amoxicillin’s Action
- Penicillin’s Specificity
- Clinical Implications
- Potential Drug Interactions: What to Expect
- Potential Interactions with Specific Penicillins
- General Advice on Combining Antibiotics
- Combining Amoxicillin and Penicillin: Risks and Benefits
- Increased Risk of Side Effects
- When a Combination Might Be Considered (Rare Cases)
- Always Consult Your Doctor
- Alternatives to Combining
- Symptoms of Adverse Reactions
- Gastrointestinal Issues
- Skin Reactions
- Other Potential Symptoms
- When to Seek Immediate Medical Help
- Note:
- When to Consult a Doctor
- Alternatives to Combined Use: Exploring Other Antibiotics
- Targeting Specific Infections
- Considerations for Alternative Antibiotics
- Beyond the Usual Suspects
Mixing Amoxicillin and Penicillin: A Detailed Guide
Don’t mix amoxicillin and penicillin. Both are antibiotics, and taking them together won’t necessarily increase effectiveness; it might even increase the risk of side effects.
Amoxicillin and penicillin are similar antibiotics, both belonging to the penicillin family. They fight bacterial infections by disrupting bacterial cell wall synthesis. Amoxicillin is a broader-spectrum antibiotic than many penicillins, meaning it’s effective against a wider range of bacteria.
Taking both simultaneously might lead to increased risk of allergic reactions, gastrointestinal distress (like nausea, diarrhea, or vomiting), or other adverse effects. The combined dosage could also place unnecessary strain on your liver and kidneys.
Always consult your doctor or pharmacist before combining medications. They can assess your specific health condition and determine the best course of treatment. Discuss any allergies or pre-existing medical conditions you have to ensure a safe treatment plan.
If you’re prescribed amoxicillin, follow your doctor’s instructions diligently concerning dosage and duration. Similarly, adhere strictly to any penicillin prescription. Completing the full course is crucial for eliminating the infection and preventing antibiotic resistance.
If you experience any unexpected or concerning side effects while taking either amoxicillin or penicillin, immediately contact your healthcare provider.
This guide provides information; it does not constitute medical advice. Always seek professional medical guidance for any health concerns.
Are Amoxicillin and Penicillin the Same?
No, amoxicillin and penicillin are not the same, although they share a family resemblance. Penicillin is a broad term encompassing many different antibiotics, while amoxicillin is a specific type of penicillin.
Think of it like this: “Penicillin” is the family name, and “Amoxicillin” is one member of that family. Amoxicillin is a semi-synthetic penicillin, meaning it’s a modified version of naturally occurring penicillin, designed to improve its properties.
Key Differences: Amoxicillin is better absorbed by the body than some other penicillins, making it a convenient oral medication. It also boasts a wider spectrum of activity against certain bacteria. However, some people may have allergic reactions to amoxicillin that they don’t experience with other penicillins. Always consult a doctor before taking any medication, particularly if you have known allergies.
If you have questions about the appropriate antibiotic for your specific health concerns, seek advice from a qualified medical professional. They can assess your individual needs and prescribe the most suitable treatment.
Understanding the Chemical Structures of Amoxicillin and Penicillin
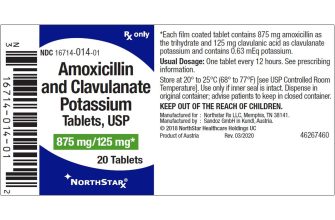
Amoxicillin and penicillin belong to the β-lactam family of antibiotics. Both share a core β-lactam ring, a four-membered cyclic amide, responsible for their antibacterial action. However, key structural differences account for their varied properties.
Amoxicillin’s Structure
Amoxicillin, chemically (2S,5R,6R)-6-[(R)-2-amino-2-(4-hydroxyphenyl)acetamido]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylic acid, adds an amino group and a hydroxyl group to the penicillin nucleus. This modification enhances its acid stability and improves its absorption in the gut.
Penicillin G’s Structure
Penicillin G (benzylpenicillin), a common penicillin, features a simpler side chain–a benzyl group–attached to the β-lactam ring. This simpler structure contributes to its susceptibility to acid degradation, limiting its oral bioavailability.
| Feature | Amoxicillin | Penicillin G |
|---|---|---|
| β-lactam ring | Present | Present |
| Side Chain | Amino group and hydroxyl group attached to a phenyl ring | Benzyl group |
| Oral Bioavailability | High | Low |
| Acid Stability | High | Low |
These structural variations explain why amoxicillin is often preferred for oral administration due to its improved absorption and acid stability compared to penicillin G. Understanding these chemical differences is key to appreciating their distinct pharmacological profiles.
Similar but Different: Mechanisms of Action
Amoxicillin and penicillin both belong to the beta-lactam family of antibiotics. They share a similar core structure, responsible for their primary mechanism of action: inhibiting bacterial cell wall synthesis. This shared mechanism explains their overlapping effectiveness against certain bacterial infections.
Amoxicillin’s Action
Amoxicillin, a broader-spectrum penicillin, blocks the formation of peptidoglycan, a vital component of bacterial cell walls. This disruption weakens the cell wall, leading to bacterial lysis and death. It achieves this by binding to penicillin-binding proteins (PBPs), key enzymes in peptidoglycan synthesis.
Penicillin’s Specificity
Penicillin, while also targeting PBPs, often exhibits a narrower spectrum of activity compared to amoxicillin. Different penicillin types show varying affinities for specific PBPs, resulting in differing bacterial targets. This accounts for their use against particular bacterial strains. The specific PBPs a penicillin type binds to dictate its effectiveness against different bacteria.
Key Difference: Amoxicillin generally has better oral bioavailability than many penicillins, meaning more of the drug enters the bloodstream after oral administration. This influences treatment decisions based on the infection’s location and severity.
Clinical Implications
Understanding these subtle differences is crucial for selecting the appropriate antibiotic. A doctor considers the specific bacteria causing the infection, the patient’s medical history, and the antibiotic’s pharmacokinetic properties before prescribing.
Potential Drug Interactions: What to Expect
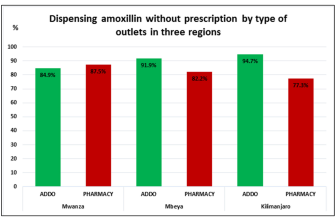
Mixing amoxicillin and penicillin isn’t typically recommended, though the risk depends heavily on the specific penicillin used and the patient’s health. Consult your doctor before combining these antibiotics.
Potential Interactions with Specific Penicillins
- Amoxicillin and Penicillin V: While both are penicillin-type antibiotics, concurrent use may increase the risk of side effects like diarrhea or nausea. Your doctor might adjust the dosage or prescribe an alternative.
- Amoxicillin and other penicillin derivatives (e.g., methicillin, oxacillin): Increased risk of side effects is possible, including allergic reactions. Close monitoring for any unusual symptoms is needed. Your doctor may opt for a different antibiotic altogether.
- Amoxicillin and penicillin-containing medications (e.g., some cough syrups): Always disclose all medications, including over-the-counter ones, to avoid unintended interactions. Double-check medication labels and consult your pharmacist if uncertain.
General Advice on Combining Antibiotics
Remember, combining antibiotics without medical supervision can lead to unexpected outcomes. These include:
- Increased risk of allergic reactions.
- Reduced effectiveness of one or both antibiotics.
- Development of antibiotic-resistant bacteria.
- Higher incidence of side effects.
Always inform your doctor or pharmacist about all your medications, including supplements and herbal remedies. This allows for careful assessment of potential interactions and helps in choosing the safest and most effective treatment plan for you. Transparency with your healthcare provider is key for your safety and well-being.
Combining Amoxicillin and Penicillin: Risks and Benefits
Generally, combining amoxicillin and penicillin is not recommended. Both are β-lactam antibiotics, meaning they work similarly and share potential side effects. Taking both simultaneously doesn’t significantly increase their effectiveness against most infections; instead, it increases your risk of adverse reactions.
Increased Risk of Side Effects
Amoxicillin and penicillin share common side effects like diarrhea, nausea, and rash. Combining them significantly raises the probability of experiencing these, and potentially more severe reactions. For example, the risk of a serious allergic reaction, like anaphylaxis, increases with higher overall β-lactam exposure.
When a Combination Might Be Considered (Rare Cases)
Very rarely, a doctor might prescribe both medications if a specific bacterial infection requires a higher antibiotic dose than a single drug provides, or if resistance to one drug exists, but not to the other. This decision requires careful consideration of the risks and benefits, usually based on specific antibiotic susceptibility testing.
Always Consult Your Doctor
Never combine amoxicillin and penicillin without explicit instructions from a physician. They’ll assess your specific situation, weigh the potential risks, and determine the appropriate course of treatment.
Alternatives to Combining
If you’re treating a bacterial infection, your doctor might consider other antibiotics from different drug classes to avoid overlapping side effects and improve the likelihood of a successful outcome.
Symptoms of Adverse Reactions
Mixing amoxicillin and penicillin can sometimes lead to adverse reactions. These reactions vary in severity, so it’s crucial to be aware of the potential symptoms.
Gastrointestinal Issues
- Nausea
- Vomiting
- Diarrhea
- Abdominal cramps
- Loss of appetite
These are common side effects and usually mild. However, severe diarrhea could indicate a more serious problem. Seek medical advice if you experience persistent or severe gastrointestinal distress.
Skin Reactions
- Rash
- Hives
- Itching
- Swelling
Skin reactions can range from mild to severe. A mild rash may clear up on its own. However, if you develop hives, significant swelling, or difficulty breathing, seek immediate medical attention as this could indicate a serious allergic reaction.
Other Potential Symptoms
- Headache
- Dizziness
- Fatigue
- Fever
These symptoms may indicate a less common reaction. While often mild, persistent symptoms warrant a doctor’s consultation.
When to Seek Immediate Medical Help
Call your doctor or go to the nearest emergency room immediately if you experience:
- Difficulty breathing or swallowing
- Swelling of your face, lips, or tongue
- Severe skin reactions
- Severe or persistent diarrhea
Note:
This information is for general knowledge and does not substitute professional medical advice. Always consult your physician or pharmacist before mixing medications.
When to Consult a Doctor
Contact your doctor immediately if you experience a severe allergic reaction, such as difficulty breathing, swelling of your face, lips, or tongue, or hives. These symptoms require immediate medical attention.
Seek medical advice if you develop diarrhea that is watery or bloody. This could indicate a serious side effect and needs prompt evaluation.
Report any new or worsening symptoms, including unusual bruising or bleeding, persistent nausea or vomiting, jaundice (yellowing of the skin or eyes), or changes in urination. These warrant further investigation.
If you experience a severe skin rash, intense itching, or blistering, contact your doctor. These could be signs of a serious reaction requiring treatment.
If you have questions about mixing amoxicillin and penicillin, or if you are unsure whether you’re experiencing a side effect, don’t hesitate to call your healthcare provider. They can provide personalized guidance based on your individual health history and medication regimen.
Alternatives to Combined Use: Exploring Other Antibiotics
If you need an alternative to combining amoxicillin and penicillin, consider cephalosporins like cefdinir or cefuroxime. These broad-spectrum antibiotics effectively treat many bacterial infections similar to those addressed by penicillin and amoxicillin. Remember to always consult your doctor for the appropriate dosage and duration.
Targeting Specific Infections
The best antibiotic choice depends heavily on the specific infection. For example, Staphylococcus aureus infections often respond well to clindamycin or linezolid. If you suspect a respiratory infection caused by atypical bacteria like Mycoplasma pneumoniae or Chlamydia pneumoniae, macrolides like azithromycin are frequently prescribed.
Considerations for Alternative Antibiotics
Drug interactions are crucial. Inform your doctor about all medications you’re currently taking, including over-the-counter drugs and supplements, before starting any new antibiotic. Allergies are another critical factor; past allergic reactions to antibiotics can indicate potential risks with similar drugs. Your physician can help determine a suitable alternative based on your medical history and current condition.
Beyond the Usual Suspects
Pseudomonas aeruginosa and other resistant bacteria require targeted treatment. Drugs like piperacillin-tazobactam or carbapenems (e.g., imipenem, meropenem) might be necessary. These are generally reserved for severe infections and require careful medical oversight.