Amoxicillin is not penicillin, but it belongs to the same family of antibiotics. Both are beta-lactam antibiotics used to treat bacterial infections. While they share a common mechanism in targeting bacterial cell walls, amoxicillin has a broader spectrum of activity and is often chosen for specific infections.
Patients frequently wonder about the relationship between these two medications, especially if they have allergies. If you are allergic to penicillin, you might also react to amoxicillin due to their structural similarities. Discuss any allergies with your healthcare provider for tailored advice and safer alternatives.
Understanding the differences helps in choosing the right treatment. Amoxicillin is typically favored for respiratory infections, while penicillin is often used for more targeted cases, like strep throat. Always consult with a healthcare professional for the best option based on your health needs.
Is Amoxicillin Penicillin?
Amoxicillin is not exactly penicillin, but it belongs to the penicillin group of antibiotics. It is a broader-spectrum antibiotic, making it effective against a wider range of bacteria.
Both amoxicillin and penicillin work by inhibiting bacterial cell wall synthesis, leading to cell lysis and death. However, amoxicillin has modifications in its chemical structure, which provide enhanced activity against certain bacteria, including some that are resistant to penicillin.
Practitioners often prescribe amoxicillin for various infections, such as respiratory tract infections, urinary tract infections, and skin infections, when penicillin alone might not suffice.
Those allergic to penicillin may also react to amoxicillin, so it’s essential to inform your healthcare provider about any known allergies. Always consult a healthcare professional for guidance on the appropriate antibiotic for your specific condition.
Understanding the Chemical Structure of Amoxicillin
Amoxicillin features a distinctive chemical structure that contributes to its antibiotic properties. It consists of a β-lactam ring fused to a thiazolidine ring. This arrangement forms the core structure characteristic of penicillins, imparting its ability to inhibit bacterial cell wall synthesis.
The molecular formula for amoxicillin is C₁₆H₁₉N₃O₅S, highlighting its composition: 16 carbon atoms, 19 hydrogen atoms, 3 nitrogen atoms, 5 oxygen atoms, and 1 sulfur atom. This complex assembly allows for a broad spectrum of antibacterial activity.
At one end of its structure, the β-lactam ring contains a carbonyl group and nitrogen atom. The carbonyl group is crucial for the mechanism of action, as it interacts with the transpeptidase enzyme in bacteria, disrupting the synthesis of peptidoglycan, a fundamental component of the bacterial cell wall.
Attached to the β-lactam ring is the thiazolidine structure, which incorporates a sulfur atom and contributes to the stability and solubility of amoxicillin in a physiological environment. The presence of a hydroxyl (-OH) group enhances its effectiveness when administered orally, improving absorption in the gastrointestinal tract.
The side chains attached to amoxicillin’s structure vary, which influences its pharmacokinetic properties and spectrum of activity. The amine (–NH₂) group increases the drug’s potency against gram-negative bacteria, distinguishing amoxicillin from other penicillins.
Understanding this chemical framework is key to grasping how amoxicillin functions in fighting infections and its effectiveness against various bacterial strains. Its structural annotations provide insight into the drug’s pharmacological behavior and therapeutic applications.
Mechanism of Action: How Amoxicillin Works
Amoxicillin targets bacterial cell walls, inhibiting their synthesis. By binding to penicillin-binding proteins (PBPs), it disrupts the cross-linking of peptidoglycan layers, a crucial component for cell wall structure. This leads to weakened cell walls, making bacteria more susceptible to osmotic pressure and eventually causing cell lysis.
This antibiotic exhibits a broad spectrum of activity. It effectively combats both gram-positive and certain gram-negative bacteria, making it versatile for treating various infections. Amoxicillin is particularly effective against Streptococcus pneumoniae and Haemophilus influenzae.
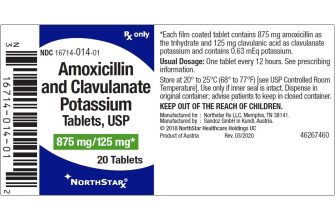
Another aspect of its action involves beta-lactamase sensitivity. While some bacteria produce enzymes that can deactivate penicillins, amoxicillin is often combined with clavulanic acid to counteract this resistance, thus enhancing its efficacy.
Amoxicillin is absorbed well when taken orally, with a bioavailability of approximately 75-90%. This maximizes the amount of active drug in the bloodstream, ensuring effective treatment with standard doses.
In summary, through its unique interaction with bacterial cell wall synthesis and strategic combinations, amoxicillin effectively treats a range of bacterial infections, making it a staple in antibiotic therapy.
Clinical Uses: When is Amoxicillin Prescribed?
Amoxicillin is commonly prescribed for various bacterial infections. Medical professionals often recommend it for the following conditions:
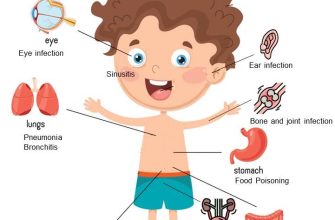
- Upper Respiratory Tract Infections: Used to treat acute otitis media, sinusitis, and pharyngitis.
- Lower Respiratory Tract Infections: Effective for pneumonia and bronchitis caused by susceptible organisms.
- Skin Infections: Treats cellulitis and other skin infections effectively.
- Urinary Tract Infections (UTIs): Often prescribed for uncomplicated UTIs.
- Gastrointestinal Infections: Utilized in treating Helicobacter pylori infection as part of a combination therapy.
Doctors may also choose amoxicillin for patients with certain risk factors. For instance:
- Patients with a history of recurrent ear infections.
- Individuals who are pregnant and require treatment for specific bacterial infections.
Amoxicillin’s broad spectrum of activity against gram-positive and some gram-negative bacteria makes it a versatile choice. Ensure appropriate usage by consulting a healthcare professional, who will consider individual health status, allergies, and local antibiotic resistance patterns before prescribing.
Allergies and Side Effects: Amoxicillin vs. Penicillin
People allergic to penicillin often experience reactions ranging from mild rashes to severe anaphylaxis. If you know you have a penicillin allergy, it’s vital to inform your healthcare provider before starting any treatment. Though amoxicillin is a penicillin derivative, cross-reactivity occurs in about 10% of cases. This means those allergic to penicillin may also react to amoxicillin, so caution is advised.
Common Side Effects
Amoxicillin often produces side effects including diarrhea, nausea, and skin rashes. These usually resolve without requiring treatment. In contrast, penicillin’s side effects can also include gastrointestinal upset and allergic reactions. Monitoring for any unusual symptoms is advisable after starting either medication.
Severe Reactions
Seek immediate medical attention if you develop symptoms such as difficulty breathing, swelling of the face or throat, or rapid heartbeat after taking either drug. These could indicate a serious allergic reaction. Always keep an open dialogue with your doctor regarding any concerns or experiences you face while on antibiotics to ensure safe treatment options.