Ciprofloxacin’s effectiveness against Group B Streptococcus (GBS) is variable. Laboratory testing remains crucial for determining susceptibility. Don’t assume sensitivity; always rely on culture and sensitivity results to guide treatment.
Minimum inhibitory concentration (MIC) values provide the most accurate assessment. An MIC ≥4 µg/mL indicates resistance; values ≤1 µg/mL suggest susceptibility. Intermediate MIC values require careful consideration of local resistance patterns and patient-specific factors.
Several factors influence GBS’s response to ciprofloxacin. These include the specific GBS strain, geographic location (influencing prevalence of resistant strains), and prior antibiotic exposure. Always consult current local antibiograms for the most reliable data on regional resistance trends.
Alternative antibiotics should be considered if ciprofloxacin resistance is suspected or confirmed. Ampicillin and penicillin remain primary choices for treating GBS infections, particularly in pregnant women. Alternative regimens may include clindamycin or vancomycin, depending on susceptibility results and clinical context. Always follow updated guidelines from infectious disease societies for optimal treatment.
- Group B Strep Ciprofloxacin Sensitivity: A Detailed Overview
- Factors Influencing Ciprofloxacin Susceptibility
- Alternative Treatment Options
- Further Investigation and Monitoring
- What is Group B Streptococcus (GBS)?
- Ciprofloxacin: Mechanism of Action and Spectrum of Activity
- Mechanism of Action Details
- Spectrum of Activity
- Gram-Positive Bacteria Sensitivity
- Intrinsic Resistance of GBS to Ciprofloxacin
- Factors Influencing GBS Ciprofloxacin Sensitivity
- Clinical Significance of Ciprofloxacin Resistance in GBS Infections
- Impact on Treatment Strategies
- Public Health Implications
- Guiding Treatment Decisions
- Alternative Treatment Options for Ciprofloxacin-Resistant GBS
- Diagnostic Methods for Determining Ciprofloxacin Sensitivity
- Prevention and Control of Ciprofloxacin-Resistant GBS
- Infection Control Measures
- Surveillance and Monitoring
- Alternative Treatment Strategies
- Public Health Initiatives
- Research and Development
- Patient Education
Group B Strep Ciprofloxacin Sensitivity: A Detailed Overview
Ciprofloxacin’s effectiveness against Group B Streptococcus (GBS) is variable and generally considered unreliable. While some strains exhibit susceptibility, many demonstrate resistance. This inconsistency necessitates reliance on susceptibility testing for each individual isolate before treatment.
Factors Influencing Ciprofloxacin Susceptibility
Resistance mechanisms in GBS include mutations in topoisomerase IV and efflux pump overexpression. These genetic variations significantly impact antibiotic efficacy. Prevalence of resistant strains varies geographically and temporally, influencing treatment success rates. Careful monitoring of local resistance patterns is critical for informed therapeutic choices. Age and underlying health conditions in the patient may also influence treatment outcomes.
Alternative Treatment Options
Penicillin remains the first-line treatment for GBS infections due to its consistently high efficacy and low resistance rates. Alternatives include ampicillin and, in penicillin-allergic patients, clindamycin or vancomycin. Always consult current antimicrobial guidelines and local resistance patterns for optimal therapy.
Further Investigation and Monitoring
Ongoing research explores novel strategies to combat GBS infections, including understanding the spread of resistance mechanisms and development of new antibiotics. Regular surveillance programs track antibiotic resistance patterns, guiding clinical practice and preventing treatment failures.
What is Group B Streptococcus (GBS)?
Group B Streptococcus (GBS), also known as Streptococcus agalactiae, is a bacterium commonly found in the vagina and rectum of healthy adults. While usually harmless to adults, GBS can cause serious infections in newborns. These infections can include pneumonia, sepsis (blood infection), and meningitis (brain infection).
Approximately 10-30% of pregnant women carry GBS. Screening for GBS during pregnancy is common and helps identify women who need preventative antibiotics during labor to protect their babies. This significantly reduces the risk of these serious infections in newborns.
GBS infections in adults are less common but can occur. These infections are more likely in people with weakened immune systems or underlying health conditions. Common manifestations include urinary tract infections and wound infections.
| Infection Type | Symptoms |
|---|---|
| Newborn Sepsis | Fever, lethargy, poor feeding, difficulty breathing |
| Newborn Pneumonia | Rapid breathing, grunting, nasal flaring |
| Newborn Meningitis | Fever, irritability, poor feeding, seizures |
| Adult UTI | Painful urination, frequent urination, cloudy urine |
| Adult Wound Infection | Pain, swelling, redness, pus |
Treatment for GBS infections typically involves antibiotics. The specific antibiotic and duration of treatment depend on the type and severity of the infection and the patient’s overall health. Prompt diagnosis and treatment are crucial for preventing serious complications.
Ciprofloxacin: Mechanism of Action and Spectrum of Activity
Ciprofloxacin targets bacterial DNA gyrase and topoisomerase IV. These enzymes are crucial for DNA replication, transcription, and repair. By inhibiting these enzymes, ciprofloxacin prevents bacterial growth and ultimately leads to bacterial cell death.
Mechanism of Action Details
Ciprofloxacin binds to these enzymes, forming a stable complex that blocks DNA replication. This mechanism differs from that of many other antibiotics, making it effective against bacteria resistant to other drug classes. The specific binding site on the enzyme determines the drug’s potency against different bacterial species.
Spectrum of Activity
Ciprofloxacin demonstrates broad-spectrum activity against a range of gram-negative bacteria, including Escherichia coli, Pseudomonas aeruginosa, and Klebsiella pneumoniae. Its effectiveness against gram-positive bacteria is generally lower, although it remains active against some strains, like Streptococcus pneumoniae. However, resistance to ciprofloxacin is a growing concern, necessitating careful consideration of antibiotic stewardship principles.
Gram-Positive Bacteria Sensitivity
Streptococcus agalactiae (Group B Strep) shows varying degrees of sensitivity to ciprofloxacin. Sensitivity testing is crucial for determining the appropriateness of this antibiotic in treating Group B Strep infections. Factors such as bacterial strain and local antibiotic resistance patterns influence the likelihood of successful treatment.
Intrinsic Resistance of GBS to Ciprofloxacin
Group B Streptococcus (GBS) exhibits inherent resistance to ciprofloxacin due to mutations in its topoisomerase IV and DNA gyrase genes. These enzymes are the targets of ciprofloxacin’s action, and alterations prevent the antibiotic from binding and inhibiting bacterial DNA replication.
This intrinsic resistance means ciprofloxacin is generally ineffective against GBS infections. Laboratory testing consistently demonstrates minimal inhibitory concentrations (MICs) significantly exceeding clinically achievable serum levels. Therefore, ciprofloxacin should not be considered a treatment option for GBS infections.
Alternative antibiotics, such as penicillin or ampicillin, are the recommended first-line treatments for most GBS infections. For penicillin-allergic patients, clindamycin or vancomycin are viable alternatives. Always consult current guidelines and antibiograms for your specific region to inform treatment choices, as antibiotic resistance patterns can vary geographically.
Monitoring antimicrobial susceptibility is key. Regular susceptibility testing remains critical to guide appropriate therapy and limit the spread of resistance.
Factors Influencing GBS Ciprofloxacin Sensitivity
Ciprofloxacin resistance in Group B Streptococcus (GBS) is a growing concern. Several factors contribute to this variation in susceptibility.
- Genetic mutations: Specific mutations in the gyrA and parC genes, encoding subunits of DNA gyrase and topoisomerase IV respectively, are primary drivers of ciprofloxacin resistance. These mutations alter the drug’s binding site, reducing its effectiveness.
- Efflux pumps: Increased expression of efflux pumps, membrane proteins that actively expel antibiotics from the bacterial cell, can significantly reduce intracellular drug concentrations, leading to resistance. Specific pumps implicated in GBS ciprofloxacin resistance include those belonging to the major facilitator superfamily (MFS).
- Porin mutations: Alterations in the structure or expression of porins, which are membrane channels that facilitate antibiotic entry into the cell, can impede ciprofloxacin uptake, contributing to resistance. Reduced porin expression decreases the amount of ciprofloxacin reaching its target.
- Exposure to other antibiotics: Prior exposure to other antibiotics, particularly fluoroquinolones or other classes with similar mechanisms, can promote the selection and spread of resistant strains via co-selection mechanisms. This includes exposure in both human and animal populations.
- Geographical location: Prevalence of ciprofloxacin resistance in GBS varies geographically. Local antibiotic prescribing practices significantly impact the selection pressure, resulting in varying resistance rates across different regions.
Understanding these factors is critical for developing effective strategies to combat GBS infections and mitigate the rise of antibiotic resistance. Regular antimicrobial susceptibility testing is essential for guiding treatment decisions.
- Regular monitoring of GBS antibiotic resistance patterns through surveillance programs is needed.
- Strict adherence to antibiotic stewardship guidelines can help curb the unnecessary use of ciprofloxacin and other antibiotics.
- Further research into the mechanisms of resistance, including the role of efflux pumps and porins, can inform the development of novel therapeutic strategies.
Clinical Significance of Ciprofloxacin Resistance in GBS Infections
Ciprofloxacin resistance in Group B Streptococcus (GBS) significantly impacts treatment choices. Rising resistance necessitates careful consideration of alternative antibiotics.
Impact on Treatment Strategies
Clinicians should avoid using ciprofloxacin empirically for GBS infections. Susceptibility testing is paramount. Penicillin remains the drug of choice for most GBS infections. However, penicillin allergies require alternative regimens, often involving aminoglycosides or clindamycin, depending on the susceptibility profile. Ampicillin remains a viable option, particularly for pregnant women with GBS colonization.
Public Health Implications
The spread of ciprofloxacin-resistant GBS strains poses a considerable challenge. Surveillance programs are needed to monitor resistance patterns and inform treatment guidelines. Implementing infection control measures in healthcare settings is vital to curb the transmission of resistant strains. This requires consistent adherence to hand hygiene protocols and appropriate antibiotic stewardship programs. Studies focusing on the genetic mechanisms driving ciprofloxacin resistance in GBS are needed for developing more effective treatment strategies.
Guiding Treatment Decisions
Before initiating treatment, always review the patient’s medical history, focusing on antibiotic allergies and prior treatments. Local antibiograms should guide treatment selections. Close monitoring of clinical response is essential, and treatment adjustments might be necessary based on culture results and clinical observations.
Alternative Treatment Options for Ciprofloxacin-Resistant GBS
For Group B Streptococcus (GBS) infections resistant to ciprofloxacin, clinicians often select alternative antibiotics based on susceptibility testing results. Penicillin remains the first-line treatment for most GBS infections, including those resistant to other antibiotics. If penicillin allergy exists, clindamycin or vancomycin are strong alternatives.
Clindamycin generally offers good activity against GBS. However, in vitro resistance is increasingly reported. Therefore, susceptibility testing is critical before prescribing clindamycin. High-dose intravenous clindamycin may be necessary for severe infections.
Vancomycin provides excellent coverage for GBS, including resistant strains. It’s typically reserved for penicillin-allergic patients or cases of clindamycin resistance. Intravenous administration is standard for severe infections, while oral vancomycin might suffice for less severe cases depending on the patient’s condition and clinical judgement.
Ampicillin combined with aminoglycosides (like gentamicin or tobramycin) represents another potent option for severe GBS infections. This combination therapy offers synergistic activity, potentially enhancing treatment success. However, aminoglycoside use should be guided by susceptibility testing and careful nephrotoxicity monitoring.
Treatment decisions require careful consideration of several factors including infection severity, patient’s clinical presentation, and local antibiogram data. Always consult with an infectious disease specialist for guidance on complex cases.
Diagnostic Methods for Determining Ciprofloxacin Sensitivity
Determining Group B Streptococcus (GBS) ciprofloxacin sensitivity relies primarily on antimicrobial susceptibility testing (AST).
- Disk Diffusion Method: This widely used method involves inoculating a Mueller-Hinton agar plate with the GBS isolate and placing a ciprofloxacin disk on the surface. After incubation, the zone of inhibition around the disk is measured and compared to standardized interpretive criteria provided by the Clinical and Laboratory Standards Institute (CLSI) or the European Committee on Antimicrobial Susceptibility Testing (EUCAST) to determine susceptibility.
- Broth Microdilution Method: This quantitative technique determines the minimum inhibitory concentration (MIC) of ciprofloxacin. A series of dilutions of ciprofloxacin is prepared in broth, and a standardized inoculum of GBS is added to each well. The MIC is the lowest concentration of ciprofloxacin that inhibits visible bacterial growth after incubation. CLSI or EUCAST guidelines define MIC breakpoints to categorize isolates as susceptible, intermediate, or resistant.
- Etest: This gradient diffusion method combines features of both disk diffusion and broth microdilution. A plastic strip containing a ciprofloxacin gradient is placed on an inoculated agar plate. After incubation, an elliptical zone of inhibition forms. The MIC is read at the intersection of the ellipse and the strip. Again, CLSI or EUCAST guidelines provide MIC breakpoints for interpretation.
Accurate results depend on several factors: proper bacterial identification, adherence to standardized protocols, use of appropriate media and reagents, and precise measurement of results. Always refer to current CLSI or EUCAST guidelines for the most up-to-date recommendations on methodology and interpretation.
- Quality control is vital; use quality control strains to ensure test accuracy.
- Report results promptly to guide appropriate antimicrobial therapy.
Prevention and Control of Ciprofloxacin-Resistant GBS
Prioritize appropriate antibiotic stewardship. Restrict ciprofloxacin use for GBS infections only when truly necessary, guided by local antibiograms showing susceptibility.
Infection Control Measures
Implement rigorous infection control practices in healthcare settings. This includes meticulous hand hygiene, consistent use of personal protective equipment (PPE), and thorough environmental cleaning and disinfection. Isolate patients with known or suspected ciprofloxacin-resistant GBS to minimize transmission.
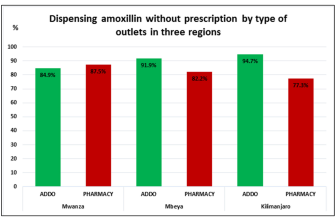
Surveillance and Monitoring
Actively monitor antibiotic resistance patterns within your institution. Regularly perform susceptibility testing on GBS isolates to track the prevalence of ciprofloxacin resistance. This data informs antibiotic selection and helps identify emerging resistance trends.
Alternative Treatment Strategies
Develop treatment guidelines emphasizing alternative antibiotics like penicillin or ampicillin for GBS infections, reserving ciprofloxacin only for cases where these are contraindicated or ineffective. Consider using combination therapy in severe infections to reduce resistance development.
Public Health Initiatives
Collaborate with public health authorities to share resistance data and coordinate strategies. Promote education and awareness among healthcare providers regarding appropriate antibiotic use and infection control for GBS.
Research and Development
Support research into novel therapeutic strategies and diagnostic tools to combat ciprofloxacin-resistant GBS. This includes exploring new antibiotics and developing rapid diagnostic tests to guide treatment decisions.
Patient Education
Educate patients about GBS infection, its risk factors, and the importance of preventive measures, especially for pregnant women. Encourage adherence to prescribed antibiotic regimens to ensure treatment efficacy.