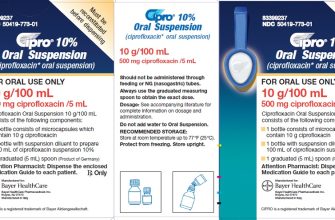
Ciprofloxacin (Cipro) isn’t typically the first-line treatment for walking pneumonia, which is usually caused by Mycoplasma pneumoniae. Doctors often prescribe macrolides like azithromycin or erythromycin instead. This is because these antibiotics are generally more effective against Mycoplasma.
However, Cipro can be an option in specific situations. If you have a severe infection or allergy to macrolides, your doctor might consider Cipro. They will also factor in the bacteria causing the infection, as Cipro is effective against some bacterial pneumonia types but not others. Always discuss treatment options with your physician.
Remember, self-treating is risky. A proper diagnosis requires a medical examination. Don’t rely on online information alone. Early diagnosis and the correct antibiotic are key to quicker recovery. Contact your doctor for an accurate assessment and a tailored treatment plan.
Important Note: This information is for educational purposes only and does not constitute medical advice. Always seek professional medical care for diagnosis and treatment of any illness.
Ciprofloxacin for Walking Pneumonia: Effectiveness and Considerations
Ciprofloxacin, a fluoroquinolone antibiotic, isn’t the first-line treatment for walking pneumonia (Mycoplasma pneumoniae infection). Macrolides like azithromycin or erythromycin are generally preferred.
Why Ciprofloxacin is Rarely Used
M. pneumoniae often demonstrates resistance to fluoroquinolones. This means Ciprofloxacin may not effectively kill the bacteria, leading to treatment failure and prolonged illness. Using an antibiotic with proven efficacy against M. pneumoniae is crucial for a timely recovery.
Situations Where Ciprofloxacin Might Be Considered
Allergy: If a patient has a severe allergy to macrolides, Ciprofloxacin could be a second-line option, but only after careful consideration of potential risks and benefits by a medical professional. Failure of other antibiotics: In rare cases, if other antibiotics fail to clear the infection, a doctor might consider Ciprofloxacin after conducting sensitivity testing to confirm its potential efficacy against the specific strain.
Important Safety Notes
Ciprofloxacin carries potential side effects, including tendonitis, tendon rupture, and peripheral neuropathy. These risks increase with age and pre-existing conditions. Discuss any potential side effects with your doctor before starting treatment. Regular monitoring is recommended during treatment to detect and manage any adverse reactions.
Always Consult a Doctor
Self-treating walking pneumonia is dangerous. A healthcare professional needs to diagnose the infection accurately and prescribe the appropriate treatment based on individual factors and the antibiotic susceptibility of the bacteria. Never use antibiotics without proper medical guidance.
Understanding Walking Pneumonia and When Ciprofloxacin Might Be Prescribed
Walking pneumonia, or atypical pneumonia, is usually caused by Mycoplasma pneumoniae or Chlamydia pneumoniae. These bacteria differ from typical pneumonia bacteria, requiring different antibiotics for effective treatment.
Ciprofloxacin, a fluoroquinolone antibiotic, isn’t the first-line treatment for walking pneumonia. Doctors typically prescribe macrolides like azithromycin or erythromycin. However, Ciprofloxacin might be considered if:
1. Allergy or Intolerance: You have a known allergy to macrolides. Your doctor will carefully assess your medical history and choose an alternative.
2. Treatment Failure: Initial treatment with macrolides proves ineffective. This situation requires a different antibiotic class. Ciprofloxacin offers an alternative in these cases, though resistance is a concern.
3. Specific Bacterial Identification: Laboratory tests confirm the presence of a different bacteria, responsive to Ciprofloxacin. This precise diagnosis necessitates a different antibiotic choice.
Important Note: Ciprofloxacin has potential side effects including tendonitis and nerve damage. Your doctor will weigh the benefits against these risks before prescribing it.
Always consult your doctor for diagnosis and treatment. Self-treating can be dangerous and delay appropriate care. They will assess your specific needs and provide the most suitable antibiotic.