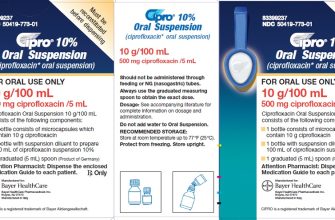
Need Ciprofloxacin? Start with understanding the dosage. Adults typically take 250-750 mg twice daily, depending on the infection. Always follow your doctor’s instructions; self-medication is risky.
Remember, Ciprofloxacin is a powerful antibiotic, and misuse can lead to antibiotic resistance. Avoid taking it unless prescribed for a bacterial infection. Viral infections, like the common cold, won’t respond to it.
Common side effects include nausea, diarrhea, and headache. Serious, though rare, reactions like tendonitis or allergic reactions require immediate medical attention. Inform your doctor about any allergies or medical conditions before starting treatment. Pregnancy and breastfeeding also necessitate careful consideration and medical guidance.
Specific concerns? Consult your physician or pharmacist. They can provide personalized advice and address your individual needs. Don’t hesitate to ask questions; clear communication is key to safe and effective treatment.
Disclaimer: This information is for educational purposes only and does not substitute professional medical advice.
Ciprofloxacin Gram-Negative Coverage: A Practical Guide
Ciprofloxacin effectively treats many gram-negative infections, but its spectrum varies. Susceptibility testing remains crucial.
Enterobacteriaceae: Ciprofloxacin generally works well against E. coli, Klebsiella pneumoniae, and Proteus mirabilis. However, resistance is increasing; always check local antibiograms.
Pseudomonas aeruginosa: Ciprofloxacin’s activity against P. aeruginosa is variable and often inadequate for serious infections. Consider alternative agents like piperacillin-tazobactam or aminoglycosides.
Haemophilus influenzae: Ciprofloxacin is usually effective, but again, local resistance patterns are critical.
Neisseria gonorrhoeae: Ciprofloxacin is no longer recommended for gonorrhea due to widespread resistance. Use ceftriaxone or other approved alternatives.
Dosage adjustments may be needed for patients with renal impairment. Always consult current guidelines and local antibiograms before prescribing Ciprofloxacin. Monitor treatment response closely.
Remember that appropriate antibiotic use helps reduce resistance development. Combine Ciprofloxacin with other antibiotics when indicated to improve treatment efficacy and avoid resistance emergence.
Ciprofloxacin Dosage and Administration: Practical Considerations
Always follow your doctor’s prescription precisely. Dosage depends heavily on the infection being treated and your individual health.
Common oral dosages range from 250mg to 750mg twice daily. Intravenous administration is used for severe infections, with dosage adjusted based on severity.
- Oral Administration: Swallow tablets whole with a full glass of water. Avoid taking with dairy products or antacids, as this can reduce absorption.
- Intravenous Administration: Administered by a healthcare professional. Infusion rate and duration vary depending on the dosage.
Duration of treatment varies, typically ranging from 7 to 14 days, but some infections may require longer therapy.
- Kidney Function: Dosage adjustments are often necessary for individuals with impaired kidney function. Your doctor will determine the appropriate dose based on your creatinine clearance.
- Age: Children’s dosages are calculated based on weight and are usually lower than adult doses.
- Other Medications: Inform your doctor about all medications you are currently taking, including over-the-counter drugs and herbal supplements, as interactions are possible.
Side effects can include nausea, diarrhea, vomiting, and abdominal pain. Report any significant side effects to your doctor immediately. Severe allergic reactions are rare but require prompt medical attention.
This information is for guidance only and does not replace professional medical advice. Always consult your doctor or pharmacist for personalized advice regarding Ciprofloxacin use.
Ciprofloxacin Resistance: Understanding and Mitigation Strategies
Reduce Ciprofloxacin use whenever possible. Prioritize alternative antibiotics where susceptibility testing indicates viability. This directly combats the development of resistance.
Implement strict infection control protocols in healthcare settings. Hand hygiene, proper sterilization techniques, and isolation procedures significantly decrease the spread of resistant bacteria. Adherence to guidelines is paramount.
Promote rational antibiotic prescribing. This involves careful consideration of patient history, clinical presentation, and local resistance patterns. Avoid broad-spectrum antibiotics when possible; instead, target specific pathogens.
Develop and implement antibiotic stewardship programs. These programs actively monitor antibiotic use, provide education to healthcare providers, and guide antibiotic selection to optimize therapy while minimizing resistance development. Regular audits and feedback mechanisms are key.
Support research and development of new antibiotics and alternative therapies. This includes exploring new drug targets, novel mechanisms of action, and alternative approaches such as bacteriophages and immunotherapy.
Enhance surveillance of antibiotic resistance. This involves actively tracking the prevalence of resistant bacteria in various settings, allowing for timely intervention and targeted public health responses. Data sharing is vital for global efforts.
Educate patients on the responsible use of antibiotics. Emphasize completing the prescribed course of antibiotics even if symptoms improve, and highlight the importance of preventing infection. Public awareness campaigns can play a vital role.
Improve diagnostics. Rapid and accurate identification of pathogens and their susceptibility profiles empowers targeted antibiotic therapy, minimizing the use of broad-spectrum agents. Investment in advanced technologies is needed.
Develop novel strategies to combat resistance. Explore innovative approaches like combination therapies, adjunctive therapies, or inhibitors of resistance mechanisms. This requires substantial investment in research and development.