For treating bacterial infections, Amoxicillin often stands out as a go-to option due to its broad-spectrum capabilities. It effectively combats a wide range of bacteria, making it suitable for conditions like pneumonia and infections of the ear, nose, and throat. However, Clindamycin HCL serves as a compelling alternative, particularly when dealing with penicillin-resistant bacteria or when patients exhibit an allergy to penicillin.
Amoxicillin works by inhibiting bacterial cell wall synthesis, which can lead to cell lysis and death. On the other hand, Clindamycin targets protein synthesis within the bacteria, disrupting their growth and reproduction. This difference in mechanism means that choosing between these antibiotics hinges on the specific type of infection and the antibiotic sensitivity of the bacteria involved.
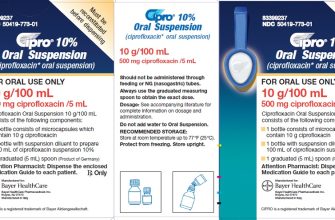
Consider the dosage forms as well; Amoxicillin is commonly available in oral tablets and liquids, making it easily accessible for various age groups. Clindamycin, while also available in oral forms, is often administered intravenously for more severe infections. Understanding these nuances will help navigate treatment options more effectively, ensuring the best outcomes for patients.
- Amoxicillin vs Clindamycin HCL: A Comprehensive Comparison
- Mechanism of Action of Amoxicillin
- Mechanism of Action of Clindamycin HCL
- Indications for Amoxicillin Use
- Indications for Clindamycin HCL Use
- Common Side Effects of Amoxicillin
- Nausea and Vomiting
- Rash and Allergic Reactions
- Common Side Effects of Clindamycin HCL
- Resistance Patterns: Amoxicillin vs Clindamycin HCL
- Choosing Between Amoxicillin and Clindamycin HCL in Clinical Practice
Amoxicillin vs Clindamycin HCL: A Comprehensive Comparison
For treating bacterial infections, amoxicillin often serves as a first-line option due to its broad-spectrum activity against various pathogens. It is effective against gram-positive bacteria and some gram-negative bacteria, making it suitable for respiratory infections, urinary tract infections, and skin infections.
On the other hand, clindamycin HCL targets anaerobic bacteria and certain protozoa. It excels in treating infections caused by organisms resistant to penicillin, making it beneficial for skin and soft tissue infections, as well as dental abscesses. Its mechanism involves inhibiting bacterial protein synthesis, which can effectively reduce inflammation and infection.
Dosage varies: amoxicillin is typically prescribed in higher doses for serious infections, while clindamycin may require careful monitoring due to potential gastrointestinal side effects, including diarrhea. Clindamycin also carries a risk of Clostridioides difficile infection, a severe type of colitis.
Both medications have shown effectiveness in treating infections, but the choice often depends on the specific type of bacteria involved and any previous antibiotic history. Patients with allergies to penicillin should consider clindamycin as a suitable alternative.
In clinical practice, clinicians often weigh the benefits and potential side effects of each medication. Selecting the appropriate antibiotic ensures optimal treatment outcomes while minimizing the risk of resistance development.
Always consult healthcare professionals for personalized advice and before starting any antibiotic treatment. Proper diagnosis and targeted therapy enhance recovery and safeguard against complications.
Mechanism of Action of Amoxicillin
Amoxicillin targets bacterial cell wall synthesis, a critical process for bacterial survival. It belongs to the penicillin group of antibiotics, inhibiting the transpeptidation enzyme, which links peptidoglycan layers together.
Key points about how Amoxicillin works:
- Inhibition of transpeptidase: Amoxicillin binds to penicillin-binding proteins (PBPs), blocking the formation of cross-links in the bacterial cell wall.
- Cell lysis: The disruption in cell wall synthesis leads to osmotic imbalance, causing the bacteria to swell and eventually burst.
- Broad-spectrum activity: Amoxicillin is effective against a variety of Gram-positive and some Gram-negative bacteria due to its ability to penetrate the outer membrane of susceptible organisms.
This antibiotic remains potent against many strains of bacteria and is often chosen for respiratory tract infections, urinary tract infections, and skin infections due to its established efficacy.
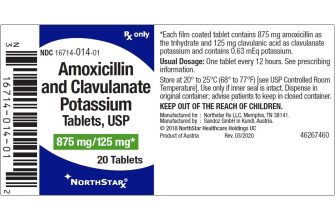
Resistance can occur, primarily through the production of beta-lactamases, enzymes that neutralize the antibiotic. Combining Amoxicillin with clavulanate can enhance its effectiveness against resistant strains.
Regular monitoring of bacterial susceptibility patterns is advisable to ensure optimal use and minimize resistance development.
Mechanism of Action of Clindamycin HCL
Clindamycin HCL operates primarily by inhibiting bacterial protein synthesis. It binds to the 50S ribosomal subunit of bacteria, disrupting the translation process essential for protein formation.
This binding prevents the peptide bond formation, effectively halting bacterial growth and multiplication. Clindamycin is particularly effective against anaerobic bacteria and certain aerobic Gram-positive organisms.
The clinical implications of clindamycin’s mechanism include:
- Combatting a variety of infections, especially those involving anaerobes.
- Providing an alternative for patients allergic to penicillin.
- Minimizing the risk of developing resistance in certain bacterial strains.
Clindamycin shows notable activity against common pathogens such as Streptococcus and Staphylococcus species. Its efficacy in treating skin and soft tissue infections is widely recognized.
For achieving optimal results, consider the dosage and duration of therapy based on the specific infection type and severity. Regular laboratory monitoring may be beneficial to assess therapeutic effectiveness and adjust treatment as needed.
Clindamycin’s mechanism highlights its role in targeted therapy, emphasizing precision in addressing infections while preserving the natural microbiota.
Indications for Amoxicillin Use
Amoxicillin is indicated for treating a range of bacterial infections. It effectively targets conditions such as streptococcal pharyngitis, commonly known as strep throat. For patients presenting respiratory tract infections like acute bronchitis or community-acquired pneumonia, amoxicillin serves as a primary choice.
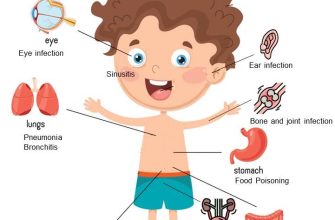
It is also utilized in managing otitis media in children and sinusitis, showcasing its efficacy against middle ear infections and sinus inflammation. Patients with urinary tract infections can benefit from amoxicillin’s antibacterial properties, providing relief from symptoms and aiding recovery.
Additionally, amoxicillin plays a crucial role in treating Helicobacter pylori infections, particularly in combination therapy for peptic ulcers. It is suitable for these cases due to its ability to penetrate gastric mucosa effectively.
For dental infections, such as periodontal abscesses, amoxicillin is often prescribed to eliminate bacterial flora contributing to the infection. Its spectrum of action extends to both gram-positive and some gram-negative bacteria, making it a versatile option for various infections.
Always consider individual patient factors, including allergies and other medications, before initiating treatment with amoxicillin. Consulting a healthcare professional for personalized advice is essential in ensuring optimal outcomes.
Indications for Clindamycin HCL Use
Clindamycin HCL is indicated for the treatment of various bacterial infections, particularly those caused by anaerobic bacteria and certain strains of staphylococci or streptococci. It is often used for skin and soft tissue infections, including cellulitis and abscesses. Additionally, dental infections such as periodontitis respond well to clindamycin therapy.
This antibiotic is also effective against some respiratory infections, such as pneumonia caused by specific bacteria. Clindamycin is recommended for patients allergic to penicillin, providing a reliable alternative treatment option. For serious bone infections, like osteomyelitis, clindamycin serves as a viable choice due to its ability to penetrate bone tissue effectively.
Furthermore, it plays a role in managing infections associated with endocarditis, particularly in patients with valvular heart disease. Clindamycin is indicated for the treatment of certain gynecological infections, including bacterial vaginosis. Its application extends to treating severe acne and various forms of sinusitis.
Always consult with a healthcare professional to ensure clindamycin is appropriate for your specific condition, ensuring safe and effective use. Regular monitoring during treatment is advisable to observe for potential side effects or adverse reactions.
Common Side Effects of Amoxicillin
Patients taking amoxicillin may experience several common side effects. These include diarrhea, which occurs in some individuals due to the antibiotic’s impact on gut bacteria. Staying hydrated and consuming easily digestible foods can help manage this symptom.
Nausea and Vomiting
Nausea and occasional vomiting may occur as the body adjusts to the medication. Taking amoxicillin with food can reduce stomach discomfort and mitigate these effects. If vomiting persists, consulting a healthcare provider is advisable.
Rash and Allergic Reactions
Some individuals may develop a mild rash or experience itching. While most rashes are harmless, any signs of severe allergic reaction, such as difficulty breathing or swelling of the face and throat, require immediate medical attention. If a rash appears, inform your doctor for further evaluation.
Common Side Effects of Clindamycin HCL
Clindamycin HCL may cause several side effects, which can vary in severity among individuals. Being aware of these effects helps in monitoring your response to the medication.
The most frequently reported side effects include gastrointestinal issues. Patients often experience nausea, vomiting, and diarrhea. Staying hydrated and consuming light meals can mitigate these symptoms. If diarrhea becomes severe or persists beyond 24 hours, consulting a healthcare provider is advisable, as this can indicate a more serious condition like Clostridium difficile infection.
Allergic reactions may also occur, presenting as rashes, itching, or swelling. Immediate medical attention is necessary if you notice difficulty breathing or swelling of the face or throat. Such reactions can indicate an anaphylactic response.
Skin-related issues are common as well. Some individuals report acne, rash, or other dermatological reactions while on Clindamycin. If any skin rash worsens or spreads, it’s important to seek medical advice promptly.
Rarely, Clindamycin can affect liver function or cause changes in blood cell counts. Routine blood tests may be recommended to monitor liver enzymes and blood parameters during prolonged therapy.
| Side Effect | Common Symptoms | Action |
|---|---|---|
| Gastrointestinal | Nausea, vomiting, diarrhea | Stay hydrated, consult doctor if severe |
| Allergic reaction | Rash, itching, swelling | Seek immediate medical help |
| Skin reactions | Acne, rash | Consult doctor if rash worsens |
| Liver function | Fatigue, jaundice | Monitor liver function with blood tests |
Understanding these side effects empowers you to manage your health effectively while using Clindamycin HCL. Always communicate openly with your healthcare provider about your experience with the medication.
Resistance Patterns: Amoxicillin vs Clindamycin HCL
Amoxicillin resistance is notably common among certain bacterial strains, particularly in Streptococcus pneumoniae and Haemophilus influenzae. Surveillance data indicate that resistance in Streptococcus pneumoniae can reach levels of up to 30%. Clindamycin, however, faces its own challenges with resistance, especially in Staphylococcus aureus, where over 25% of isolates show resistance patterns.
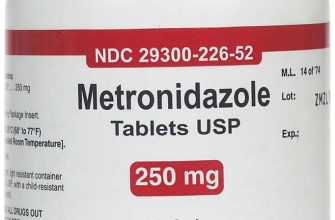
When selecting between these antibiotics, consider the specific pathogens involved. For respiratory tract infections caused by Staphylococcus aureus, clindamycin can be a superior choice, especially in cases where penicillin resistance is a concern. Resistance mechanisms for amoxicillin include the production of beta-lactamase enzymes, while clindamycin resistance often arises from target site modifications through erm genes or efflux pumps.
In mixed bacterial infections, susceptibility testing helps inform the choice of antibiotic. Clindamycin effectively targets anaerobic bacteria, making it preferable in treating conditions like oral infections and abscesses. Continuous monitoring of resistance patterns in your local area can guide effective treatment decisions.
Ultimately, understanding these resistance patterns directs clinicians towards appropriate antibiotic choices, ensuring better patient outcomes and effective management of infections.
Choosing Between Amoxicillin and Clindamycin HCL in Clinical Practice
Select amoxicillin for common bacterial infections, particularly those caused by streptococci and some staphylococci. It’s a broad-spectrum penicillin, effective against a range of pathogens and typically well-tolerated. Use it for respiratory tract infections, otitis media, and urinary tract infections. Monitor for allergic reactions, which may occur in patients with penicillin allergies.
Opt for clindamycin HCL when dealing with anaerobic infections or when patients are allergic to penicillin. Clindamycin targets certain strains of staphylococci and is effective against some gram-positive organisms. It’s particularly useful for skin infections, dental infections, and when treating serious infections caused by anaerobic bacteria. Be cautious of potential gastrointestinal side effects, including antibiotic-associated colitis.
Evaluate the site of infection and the likely organisms involved. Conduct sensitivity testing when necessary to ensure the chosen antibiotic will be effective. Review patient history for allergies and previous antibiotic usage, as this affects treatment choices. Consider the pharmacokinetics of each drug; amoxicillin has better absorption when taken with food, while clindamycin can be taken without regard to meals.
Always balance the choice of antibiotic with the risk of developing resistance. Amoxicillin is widely prescribed, which may lead to increased resistance. Clindamycin can be a valuable alternative in cases where resistance is a concern. Tailor your approach based on local resistance patterns, ensuring effective treatment while minimizing the risk of adverse outcomes.
Finally, educate patients about their treatment. Inform them of potential side effects and the importance of completing the prescribed course even if symptoms improve. Empower them to recognize signs of allergic reactions or severe gastrointestinal issues, prompting immediate medical attention if necessary.