If you’re deciding between amoxicillin and azithromycin for treating bacterial infections, understanding their differences can steer you towards the right choice. Amoxicillin is typically preferred for infections like strep throat and some types of pneumonia, while azithromycin is often more effective against respiratory infections and sexually transmitted infections.
Amoxicillin, a penicillin-type antibiotic, works by inhibiting the growth of bacteria. It’s generally well-tolerated, but some individuals may experience allergic reactions. On the other hand, azithromycin, a macrolide antibiotic, has a broader spectrum of activity against tougher bacterial pathogens and is often prescribed for patients who have penicillin allergies.
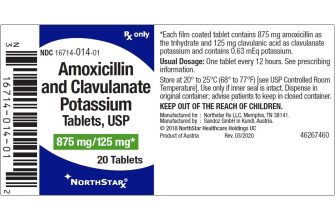
When it comes to dosage, amoxicillin is commonly taken multiple times a day for a week, while azithromycin may only require a shorter course due to its long half-life. This difference can enhance patient adherence, making azithromycin an attractive option for those who prefer fewer doses. Always consult your healthcare provider to determine which antibiotic aligns with your specific health needs and any potential interactions with other medications.
- Amoxicillin vs Azithromycin: A Comprehensive Comparison
- Mechanism of Action
- Side Effects and Considerations
- Mechanism of Action: How Each Antibiotic Works
- Clinical Uses: When to Prescribe Amoxicillin vs Azithromycin
- Azithromycin’s Role
- Combination Therapy
- Side Effects and Contraindications: Understanding Risks
- Resistance Patterns: Addressing Antimicrobial Resistance Issues
- Amoxicillin Resistance
- Azithromycin Resistance
Amoxicillin vs Azithromycin: A Comprehensive Comparison
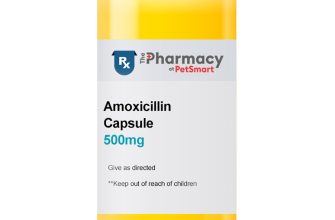
Choose amoxicillin for bacterial infections like pneumonia, bronchitis, and urinary tract infections. This penicillin derivative has a broad spectrum, targeting various bacteria effectively. It’s often the drug of choice for pediatric infections due to its safety profile and ease of administration.
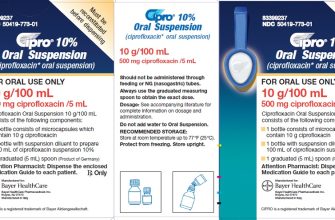
Azithromycin, on the other hand, excels in respiratory infections and atypical bacterial infections, including those caused by Chlamydia and Mycoplasma. Its unique pharmacokinetics allow for once-daily dosing and shorter treatment courses. This makes it convenient for patients who may struggle with adherence to longer regimens.
Mechanism of Action
Amoxicillin works by inhibiting bacterial cell wall synthesis, leading to cell lysis and death. This action is particularly effective against Gram-positive bacteria. Azithromycin inhibits bacterial protein synthesis by binding to the 50S ribosomal subunit, providing a bacteriostatic effect. This makes azithromycin suitable for infections caused by organisms resistant to other antibiotics.
Side Effects and Considerations
Common side effects of amoxicillin include gastrointestinal disturbances, such as diarrhea and nausea. An allergic reaction, although rare, can occur, particularly in patients with a penicillin allergy. Azithromycin may cause abdominal pain, diarrhea, and potential cardiac arrhythmias in susceptible individuals. It’s essential to consider patient allergies and comorbidities when selecting either drug.
Consult a healthcare provider for personalized advice based on individual health circumstances and the specific nature of the infection. Each medication has its strengths and ideal scenarios for use, tailoring treatment to enhance outcomes.
Mechanism of Action: How Each Antibiotic Works
Amoxicillin and azithromycin are two powerful antibiotics, each employing distinct mechanisms to combat bacterial infections effectively. Understanding how they function helps in their optimal use.
Amoxicillin operates by inhibiting bacterial cell wall synthesis. It binds to specific penicillin-binding proteins (PBPs) located inside the bacterial cell wall, which are crucial for the final stages of cell wall assembly. This binding disrupts the transpeptidation process, leading to cell lysis and eventual death of the bacteria. Amoxicillin predominantly targets Gram-positive bacteria and some Gram-negative bacteria, making it suitable for treating infections such as ear infections, throat infections, and urinary tract infections.
In contrast, azithromycin works through a different pathway. It binds to the 50S subunit of the bacterial ribosome, inhibiting protein synthesis. By obstructing the peptide bond formation during translation, azithromycin prevents bacteria from growing and reproducing. This action is particularly effective against a wider range of pathogens, including atypical bacteria and some Gram-negative bacteria. Azithromycin is often utilized for respiratory tract infections, skin infections, and sexually transmitted diseases.
| Antibiotic | Mechanism of Action | Target Bacteria | Common Uses |
|---|---|---|---|
| Amoxicillin | Inhibits cell wall synthesis | Gram-positive, some Gram-negative | Ear infections, throat infections, urinary tract infections |
| Azithromycin | Inhibits protein synthesis | Atypical bacteria, Gram-negative | Respiratory infections, skin infections, STDs |
Both antibiotics are effective but work differently; their specific mechanisms illustrate their respective strengths and clinical applications. Choose the appropriate treatment based on the type of infection and bacterial susceptibility.
Clinical Uses: When to Prescribe Amoxicillin vs Azithromycin
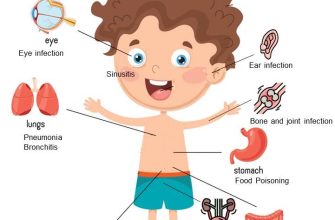
Use amoxicillin primarily for treating infections caused by susceptible bacteria. This includes conditions like otitis media, sinusitis, and certain types of pneumonia. Amoxicillin is effective against common organisms such as Streptococcus pneumoniae and Haemophilus influenzae. It works well for uncomplicated urinary tract infections and skin infections, providing reliable coverage.
In cases of respiratory infections, such as bronchitis or mild bacterial pneumonia, amoxicillin is often the preferred choice, especially when Streptococcus is likely. For patients with a history of penicillin allergy, alternative antibiotics may be considered.
Azithromycin’s Role
Prescribe azithromycin for atypical bacterial infections, such as those caused by Chlamydia pneumoniae, Mycoplasma pneumoniae, and Legionella pneumophila. It’s particularly useful in treating community-acquired pneumonia where atypical pathogens are involved. Azithromycin also effectively targets sexually transmitted infections, including chlamydia and gonorrhea.
This antibiotic excels in treating respiratory infections, especially in patients with COPD or asthma. It is commonly used in patients with a confirmed allergy to penicillin, as it is generally well-tolerated.
Combination Therapy
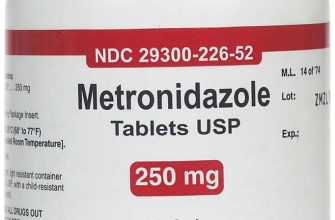
In certain situations, both antibiotics may be combined, particularly in severe pneumonia where polymicrobial infection is suspected. This approach ensures broad coverage while addressing the potential for resistance. Always assess local guidelines to optimize therapy based on susceptibility patterns.
In summary, select amoxicillin for typical bacterial infections, especially in children and uncomplicated cases. Reserve azithromycin for atypical pathogens and specific infections where it shines. Tailor your choice based on the patient’s medical history and local resistance data.
Side Effects and Contraindications: Understanding Risks
Amoxicillin can cause side effects including nausea, vomiting, diarrhea, and allergic reactions such as rash or itching. The most severe reactions may involve anaphylaxis, a life-threatening condition requiring immediate medical attention.
Common side effects of azithromycin include gastrointestinal upset like diarrhea, nausea, and abdominal pain. Less frequently, it can lead to allergic reactions or liver problems, which may present as jaundice or dark urine. Serious heart symptoms, such as irregular heartbeat, can also occur, prompting a consultation with a healthcare provider.
Amoxicillin carries specific contraindications. Patients with a known allergy to penicillin or cephalosporins should avoid its use. Individuals with mononucleosis, renal issues, or those taking methotrexate must approach treatment with caution.
Azithromycin poses risks for patients with known hypersensitivity to macrolide antibiotics. It is best avoided in individuals with existing heart conditions or those taking medications that may interact, including certain antiarrhythmics.
Always consult healthcare professionals before making decisions related to the use of these antibiotics. Monitoring for any adverse reactions during treatment can enhance safety and efficacy in managing infections.
Resistance Patterns: Addressing Antimicrobial Resistance Issues
Monitor resistance patterns regularly to guide appropriate antibiotic usage. Understanding local epidemiology helps in selecting the most effective treatment for infections. Both amoxicillin and azithromycin face growing resistance, impacting their utility in clinical settings.
Amoxicillin Resistance
Amoxicillin commonly encounters resistance from:
- Streptococcus pneumoniae: Increasing rates of penicillin-resistance make susceptibility testing crucial.
- Escherichia coli: Resistance primarily due to plasmid-mediated beta-lactamases.
- Haemophilus influenzae: Some strains produce beta-lactamases, conferring resistance at significant levels.
Regular sensitivity testing can help identify effective antibiotics and guide treatment decisions. Avoid overprescribing amoxicillin to mitigate resistance development.
Azithromycin Resistance
Resistance to azithromycin is on the rise, particularly in:
- Streptococcus pneumoniae: Resistance primarily linked to efflux pumps and methylation of the target site.
- Neisseria gonorrhoeae: The emergence of high-level resistance is alarming and influences treatment protocols.
- Mycoplasma genitalium: Resistance markers require monitoring to ensure effective management.
Selecting antibiotics based on susceptibility data can lead to better outcomes. Engage in stewardship programs to encourage appropriate prescribing practices. Encourage collaboration among healthcare providers to share resistance data and reinforce treatment guidelines.