If you have an amoxicillin allergy, using Rocephin (ceftriaxone) can be a suitable alternative. This cephalosporin antibiotic does not share the same beta-lactam structure as amoxicillin, reducing the risk of cross-reactivity. Always inform your healthcare provider about your allergies before starting any new medication.
Monitor for allergic reactions if you begin Rocephin. Symptoms can include rash, itching, or difficulty breathing. If you experience any of these, discontinue use and seek immediate medical attention. It’s essential to follow your healthcare provider’s instructions regarding dosage and duration to ensure safety and effectiveness.
Throughout your treatment, maintain open communication with your healthcare professional. If you have any concerns or experience unexpected side effects, they can adjust your treatment plan as needed. Documentation of your allergy is crucial for future medical care, so ensure that all healthcare providers are aware of your amoxicillin allergy.
- Understanding Rocephin Use for Patients with Amoxicillin Allergy
- Clinical Considerations for Prescribing Rocephin
- Assessing Renal Function
- Potential Drug Interactions
- Identifying Alternatives and Cross-Reactivity Risks
- Alternatives to Amoxicillin
- Understanding Cross-Reactivity Risks
- Patient Management Strategies for Amoxicillin-Allergic Individuals
- Alternative Antibiotic Selection
- Allergy Documentation and Communication
Understanding Rocephin Use for Patients with Amoxicillin Allergy
For patients with an amoxicillin allergy, Rocephin (ceftriaxone) serves as a safe alternative for treating various infections. Rocephin belongs to the cephalosporin class of antibiotics, which typically demonstrates a different allergy profile compared to penicillin-based drugs.
Before prescribing Rocephin, healthcare providers assess the severity of the amoxicillin allergy. In most cases, Rocephin can be administered safely if the patient does not have a documented severe anaphylactic reaction to penicillin. Those with reactions limited to mild rashes may still use Rocephin without issue.
Monitoring for any adverse reactions after administration is important, especially in patients with a history of multiple drug allergies. Symptoms such as rash, itching, or difficulty breathing require immediate medical attention.
Dosage of Rocephin often varies based on the infection being treated. Typical adult doses range from 1 to 2 grams, given intravenously or intramuscularly, once daily. Pediatric dosing is based on weight and specific clinical indications.
Patients should maintain an open line of communication with their healthcare provider. Reporting any unexpected side effects or symptoms after taking Rocephin can help ensure safety and effectiveness during treatment.
In summary, Rocephin is a viable treatment option for patients allergic to amoxicillin, provided careful evaluation and monitoring are in place. This approach minimizes risks and promotes effective infection management.
Clinical Considerations for Prescribing Rocephin
Begin with a thorough patient history to identify any allergies, specifically to penicillin derivatives. Rocephin (ceftriaxone) is a cephalosporin antibiotic and may be prescribed to patients with an amoxicillin allergy, as cross-reactivity is generally low. However, individual assessments are necessary.
Assessing Renal Function
Evaluate renal function before initiation. Ceftriaxone is predominantly excreted through the kidneys, and dosage adjustments are essential in patients with impaired renal function to prevent toxicity. Monitor creatinine levels throughout the treatment regimen.
Potential Drug Interactions
Review patient medications for potential interactions. Rocephin may enhance the effects of anticoagulants or other drugs metabolized by the liver. Regular monitoring of INR may be warranted for patients on anticoagulation therapy. In addition, avoid co-administration with calcium-containing solutions due to the risk of precipitation, especially in neonates.
Provide clear counseling about possible side effects, such as gastrointestinal disturbances or allergic reactions, and instruct patients to report any unusual symptoms promptly. This proactive approach can significantly enhance patient safety and treatment outcomes.
Identifying Alternatives and Cross-Reactivity Risks
If a patient is allergic to amoxicillin, it is crucial to identify suitable alternatives while considering the risk of cross-reactivity. Rocephin (ceftriaxone) is often used in such cases, yet understanding the safety of its use is vital.
Alternatives to Amoxicillin
- Cefdinir: This cephalosporin antibiotic can be a suitable alternative for treating various infections.
- Clindamycin: Especially effective for skin and soft tissue infections, it is a good option if the infection is anaerobic.
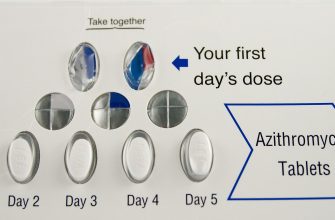
- Azithromycin: This macrolide antibiotic is beneficial for respiratory infections and is a safe choice for those with amoxicillin allergy.
- Metronidazole: For anaerobic infections, especially in oral or abscess cases, this antibiotic works well without cross-reactivity concerns.
Understanding Cross-Reactivity Risks
Cross-reactivity between penicillins and cephalosporins can pose a risk, particularly with first-generation cephalosporins. Rocephin is classified as a third-generation cephalosporin, generally considered safer for individuals with penicillin allergies.
- Incidence of Cross-Reactivity: Studies reveal that the cross-reactivity rate is significantly lower with second- and third-generation cephalosporins, estimated at 1% or less.
- Assessing Allergy Severity: A detailed allergy history is essential. Focus on the type of reaction (e.g., rash, anaphylaxis) to help determine safety.
- Skin Testing: Consider performing skin tests for high-risk patients before administering Rocephin to confirm tolerability.
Always consult a healthcare provider for personalized advice and to determine the best antibiotic choice tailored to individual allergy profiles.
Patient Management Strategies for Amoxicillin-Allergic Individuals
Ensure thorough medical history intake, focusing on specific reactions to amoxicillin. Encourage patients to provide detailed descriptions of symptoms, including onset and severity. Develop a clear understanding of whether the allergy involved anaphylaxis or non-life-threatening reactions.
Alternative Antibiotic Selection
Utilize antibiotics that have a lower risk of cross-reactivity with penicillins. Consider options such as cefdinir, cefuroxime, or azithromycin for treating infections. Discuss these alternatives with the patient, highlighting the importance of avoiding amoxicillin to prevent any allergic reactions.
Allergy Documentation and Communication
Document the allergy clearly in the patient’s medical records. Use allergy alerts in electronic health records to notify all healthcare providers. Provide patients with an allergy card that details their amoxicillin allergy, which they can carry at all times for reference during emergencies.
Educate patients about recognizing and managing allergic reactions. Instruct them on the signs of severe reactions, emphasizing the importance of seeking immediate medical attention. Discuss the potential use of an epinephrine auto-injector for those with a history of anaphylaxis.
Schedule regular follow-ups to assess the patient’s health status and review any new medications. Provide an open environment where patients feel comfortable discussing their concerns related to antibiotic use and allergy management.