Monitor patients for signs of allergic reactions, including rash, itching, and difficulty breathing, especially during the first doses. Administer amoxicillin with food to reduce gastrointestinal upset, ensuring optimal absorption and patient comfort. Maintain accurate documentation of dosage and timing to establish a clear medication history.
Educate patients about the importance of completing the full course of amoxicillin, even if symptoms improve. Discuss potential side effects, such as nausea and diarrhea, and encourage the intake of probiotics to help mitigate gastrointestinal disturbances. Regularly assess renal function in patients, particularly those with pre-existing conditions, to prevent complications.
Evaluate patient response to therapy through symptom resolution and laboratory results. Engage with healthcare teams to ensure appropriate adjustments based on individual patient needs. Encourage hydration to facilitate the excretion of the drug and prevent dehydration, especially in cases of diarrhea.
- Nursing Interventions for Amoxicillin
- Monitoring Patient Allergies to Amoxicillin
- Documentation and Alerts
- Patient Education and Communication
- Assessing Therapeutic and Adverse Effects of Amoxicillin
- Educating Patients on Amoxicillin Administration
- Administration Guidelines
- What to Avoid
- Implementing Infection Control Practices with Amoxicillin
- Documenting Patient Responses to Amoxicillin Treatment
- Coordinating Follow-Up Care Post Amoxicillin Therapy
- Monitor for Secondary Infections
- Evaluate Medication Adherence
Nursing Interventions for Amoxicillin
Monitor the patient for signs of an allergic reaction. This includes observing for symptoms such as rash, itching, swelling, or difficulty breathing within the first few doses of amoxicillin.
Assess the patient’s renal function prior to initiating therapy, particularly in those with pre-existing kidney issues. Adjust doses accordingly based on renal function tests.
Educate the patient about the importance of completing the full course of amoxicillin, even if symptoms improve. This prevents antibiotic resistance.
Instruct the patient to take amoxicillin with food to reduce gastrointestinal upset. This helps improve tolerance and absorption.
Advise on potential drug interactions. For example, warn against the concurrent use of methotrexate and probenecid, as they may affect amoxicillin’s efficacy.
- Encourage regular hydration to support kidney function.
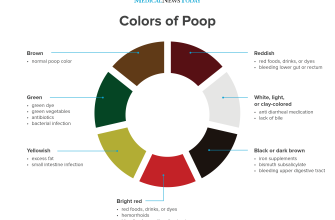
- Monitor for gastrointestinal side effects such as diarrhea, and advise on dietary adjustments as needed.
- Check for superinfection signs, such as oral thrush or vaginal yeast infections, particularly in patients on prolonged therapy.
Document the administration and any side effects observed during treatment. This ensures continuity of care and enhances patient safety.
Provide guidance on the possibility of staining teeth in children and the importance of oral hygiene.
Evaluate the effectiveness of therapy by monitoring clinical symptoms and laboratory results. Adjust treatment plans based on outcomes.
Communicate with the healthcare team regarding any adverse reactions or complications experienced by the patient. Collaborative care improves patient safety and outcomes.
Monitoring Patient Allergies to Amoxicillin
Assess patient allergies before administering amoxicillin. Review the patient’s medical history for documented allergies. Ask detailed questions about reactions to penicillin or other beta-lactam antibiotics, noting symptoms such as rash, swelling, or difficulty breathing.
Documentation and Alerts
Document all allergy information in the electronic health record (EHR). Set alerts for healthcare team members to ensure they are aware of these allergies. Include specific details about the type of reaction experienced. This proactive approach minimizes the risk of administering amoxicillin to allergic patients.
Patient Education and Communication
Discuss potential allergic reactions with patients and their families. Provide clear information on symptoms to watch for after administration. Encourage patients to report any adverse effects immediately. Empower them with knowledge about their allergies and the importance of avoiding certain medications.
Conduct regular reviews of the patient’s medication lists to identify any potential cross-reactivity with other medications. This vigilance supports safe prescribing practices and enhances patient safety.
Assessing Therapeutic and Adverse Effects of Amoxicillin
Monitor the patient’s response to amoxicillin, focusing on therapeutic outcomes such as resolution of infection symptoms. Common conditions treated with amoxicillin include otitis media, sinusitis, and pneumonia. Examine for symptom improvement, such as reduced fever, decreased pain, or clearance of respiratory distress.
Regularly assess vital signs, including temperature, heart rate, and respiratory rate, to evaluate the effectiveness of treatment. Document any changes in the patient’s condition, particularly the onset of new symptoms.
Be vigilant for adverse effects associated with amoxicillin. Common side effects include gastrointestinal disturbances like diarrhea, nausea, and vomiting. Notify healthcare providers if these symptoms occur, especially if they are severe or persistent.
Monitor for signs of allergic reactions, such as rash, itching, or difficulty breathing. Ensure that patients are aware of possible allergy symptoms and know when to seek medical attention. Assess liver and renal function tests to identify potential impacts of the medication on these organs.
| Assessment Focus | Indicators of Effectiveness | Adverse Effects to Monitor |
|---|---|---|
| Symptom Resolution | Reduction in fever, pain relief | Diarrhea, nausea, vomiting |
| Vital Signs | Stable heart rate, normal temperature | Allergic reactions (rash, itching) |
| Patient Feedback | Improved well-being, energy levels | Signs of liver or kidney issues |
Document all findings meticulously. Sharing this information with the healthcare team facilitates timely interventions for any adverse effects and ensures continuous evaluation of the treatment’s effectiveness.
Educating Patients on Amoxicillin Administration
Take amoxicillin exactly as prescribed by your healthcare provider. This typically means following the specified dosage and timing to maximize its effectiveness. Do not skip doses, and if you miss one, take it as soon as you remember. If it’s close to your next dose, skip the missed dose and continue with your regular schedule.
Administration Guidelines
- Amoxicillin can be taken with or without food. For some patients, taking it with food may reduce stomach upset.
- Always use the measuring device provided with your medication to ensure accurate dosing.
- Shake the liquid formulation well before measuring to ensure proper mixing of the medication.
- Store amoxicillin at room temperature and out of direct sunlight. Do not refrigerate unless instructed to do so.
What to Avoid
- Avoid taking any antacids that contain aluminum or magnesium within two hours of taking amoxicillin, as they can interfere with absorption.
- Do not combine amoxicillin with alcohol. Drinking alcohol can increase side effects and diminish the effectiveness of the antibiotic.
- If allergic reactions occur, such as rash or difficulty breathing, seek medical attention immediately.
Complete the full course of amoxicillin, even if you start feeling better before finishing the medication. This helps prevent antibiotic resistance and ensures that the infection is fully treated.
Communicate any side effects, such as diarrhea or stomach discomfort, to your healthcare provider, as they may need to monitor your condition closely. Regular follow-ups may be necessary to assess the treatment’s effectiveness.
Implementing Infection Control Practices with Amoxicillin
Administer amoxicillin with clear guidelines on dosage and timing to enhance its efficacy. Patients should follow a strict regimen, taking the medication at evenly spaced intervals, ideally at the same time each day. This practice helps maintain stable drug levels in the bloodstream.
Encourage good hygiene practices among patients, including regular handwashing and cleaning of potentially contaminated surfaces. These actions significantly reduce infection transmission, particularly in settings like hospitals or clinics where immunocompromised individuals may be present.
Monitor for signs of infection improvement, such as decreased fever and reduced pain, while also being alert for any potential adverse reactions. This vigilance allows for timely intervention if side effects occur, ensuring patient safety and adherence to treatment.
Provide education on completing the full course of amoxicillin, even if symptoms improve. Abandoning treatment early may lead to antibiotic resistance, complicating future infections. Reinforce the message that finishing the entire prescription is crucial for recovery.
Advocate for routine assessments of the patient’s condition, encouraging follow-up appointments to evaluate the effectiveness of the antibiotic and make necessary adjustments. This ongoing evaluation enhances treatment outcomes and allows healthcare providers to adapt strategies based on the patient’s progress.
Finally, emphasize the importance of communication between patients and healthcare providers. Patients should feel comfortable reporting any side effects or concerns. Open dialogue fosters trust and allows for more personalized care, further supporting infection control efforts.
Documenting Patient Responses to Amoxicillin Treatment
Record the patient’s response to amoxicillin promptly after each dose. Note any side effects encountered, such as gastrointestinal issues or allergic reactions. Document specific symptoms, including severity and duration, to track tolerance levels and assess the need for adjustments.
Assess vital signs regularly, especially in the initial days of treatment. Changes in temperature, heart rate, or blood pressure can indicate an adverse reaction. Make detailed entries in the medical record about any significant changes observed.
Engage with the patient to gather feedback on their health status. Ask about symptom relief and any new symptoms that may arise. Use this information to evaluate the effectiveness of the treatment. Encourage patients to articulate their experiences, ensuring their concerns are well-documented.
Monitor laboratory results, particularly if the patient is on amoxicillin for an extended period. Pay attention to renal function tests and liver enzymes, as these can indicate the medication’s impact on organ systems. Document relevant laboratory values and correlate them with the treatment course.
If the patient shows signs of improvement, such as decreased fever or improved functioning, capture these changes in the chart. Highlight any milestones in recovery, as this provides valuable insight into the medication’s efficacy.
Maintain clear documentation for future reference and continuity of care. Include dosage details, duration of treatment, and any changes to therapy. This information aids other healthcare providers in understanding the patient’s history with amoxicillin.
Always ensure that patient interactions and responses are documented in a timely manner. Accurate records support effective communication among healthcare team members and enhance patient safety.
Coordinating Follow-Up Care Post Amoxicillin Therapy
Schedule a follow-up appointment within one to two weeks after completing amoxicillin therapy. During this visit, assess the patient’s response to treatment. Evaluate for signs of infection resolution, such as symptom improvement and laboratory results. Document any adverse reactions experienced during the course of medication, particularly gastrointestinal issues or allergic reactions.
Monitor for Secondary Infections
Encourage patients to report any new symptoms that may arise after treatment. Assess for signs of secondary infections, especially if the initial infection was bacterial in nature. Educate patients about the potential for yeast infections following antibiotic use. Consider scheduling a follow-up visit specifically for women to monitor for these complications.
Evaluate Medication Adherence
Discuss adherence to the prescribed amoxicillin regimen. Address any challenges the patient faced, such as misunderstanding instructions or side effects that hindered compliance. Reinforce the importance of completing the full course of antibiotics, even if symptoms improve. Provide written materials to reinforce proper medication use and address any lingering questions.
Collaborate with pharmacists to review any additional medications the patient may be taking for potential interactions. This step enhances patient safety and ensures a balanced approach to further treatment options. Document all findings and adjustments made during the follow-up visit to create a complete patient care profile.