Ciprofloxacin (Cipro) is not a recommended treatment for MRSA infections. MRSA, or methicillin-resistant Staphylococcus aureus, is resistant to many common antibiotics, including Cipro. Using Cipro against MRSA is unlikely to be effective and could contribute to further antibiotic resistance.
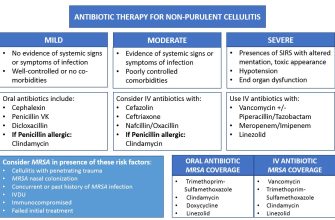
Instead of Cipro, treatment typically involves antibiotics like vancomycin, linezolid, daptomycin, or ceftaroline. Your doctor will determine the best antibiotic based on your specific infection, its severity, and your medical history. Factors like the location of the infection and any allergies you have also play a role in selecting the appropriate treatment.
Always consult your physician or other qualified healthcare professional for diagnosis and treatment of MRSA. They can perform tests to confirm the infection and prescribe the most appropriate and effective antibiotic. Self-treating can be dangerous and delay proper care.
Early diagnosis and appropriate antibiotic treatment are key to successfully managing MRSA infections. Delaying treatment can lead to complications and a prolonged recovery period. Listen to your body, and seek medical attention if you suspect an MRSA infection.
- Cipro for MRSA: A Detailed Overview
- Understanding MRSA and its Resistance to Antibiotics
- Ciprofloxacin (Cipro): Mechanism of Action and Spectrum of Activity
- Mechanism of Action Details
- Spectrum of Activity
- MRSA Considerations
- Factors Influencing Activity
- Efficacy of Ciprofloxacin against MRSA: Clinical Evidence
- Limitations of Ciprofloxacin in Treating MRSA Infections
- Resistance Mechanisms
- Clinical Implications
- Alternative Treatment Options for MRSA Infections
- Surgical Debridement and Drainage
- Other Antibiotic Options
- When to Consider Ciprofloxacin for MRSA-Related Conditions
- Preventing MRSA Infections and the Role of Antibiotic Stewardship
- Antibiotic Stewardship: Your Role
- Hospital and Healthcare Settings
Cipro for MRSA: A Detailed Overview
Ciprofloxacin (Cipro) is generally ineffective against MRSA (methicillin-resistant Staphylococcus aureus).
MRSA bacteria have developed resistance to many antibiotics, including fluoroquinolones like Cipro. This resistance mechanism often renders Cipro unable to kill or inhibit the growth of MRSA. Therefore, Cipro is not a recommended treatment for MRSA infections.
Doctors rely on alternative antibiotics like vancomycin, daptomycin, linezolid, or ceftaroline for treating MRSA. The specific choice depends on factors such as the severity of the infection, the patient’s medical history, and the results of susceptibility testing.
Susceptibility testing identifies which antibiotics are most likely to be effective against a specific bacterial strain. This test is critical for determining appropriate MRSA treatment. Never self-medicate; always consult a doctor for diagnosis and treatment of any infection.
Using ineffective antibiotics contributes to the development of antibiotic resistance. Incorrect antibiotic use can prolong illness and increase the risk of serious complications. Always follow your doctor’s instructions regarding medication.
If you suspect an MRSA infection, seek immediate medical attention. Prompt diagnosis and appropriate treatment are vital for successful recovery.
Understanding MRSA and its Resistance to Antibiotics
MRSA, or methicillin-resistant Staphylococcus aureus, is a bacterium responsible for various infections, ranging from skin infections to life-threatening conditions like pneumonia and bloodstream infections. Its resistance stems from a genetic mutation affecting penicillin-binding proteins, rendering many common antibiotics ineffective.
Methicillin, a type of penicillin, was initially effective against S. aureus. However, the overuse and misuse of antibiotics fueled the development of methicillin resistance. This resistance mechanism spread rapidly, making many common antibiotics useless against MRSA. This means infections require stronger, often more toxic, treatments.
Resistance mechanisms beyond methicillin resistance are also developing. S. aureus demonstrates remarkable adaptability, developing resistance to other antibiotics like fluoroquinolones (including ciprofloxacin) and aminoglycosides. This ongoing evolution necessitates careful antibiotic stewardship and infection control measures.
S. aureus acquires resistance through genetic mutations and horizontal gene transfer. Mutations directly alter the bacterial structure, reducing antibiotic effectiveness. Horizontal gene transfer involves the sharing of resistance genes between bacteria, accelerating the spread of resistance across strains.
Consequences of resistance include prolonged illness, increased healthcare costs, and higher mortality rates. Effective infection control, including proper hand hygiene and wound care, is key to preventing the spread of MRSA. Antibiotic use should always be guided by a healthcare professional and strictly adhere to prescribed regimens to minimize resistance development. Careful selection of antibiotics based on susceptibility testing is crucial to successful treatment.
Ciprofloxacin (Cipro): Mechanism of Action and Spectrum of Activity
Ciprofloxacin inhibits bacterial DNA gyrase and topoisomerase IV, enzymes crucial for bacterial DNA replication, transcription, repair, and recombination. This inhibition prevents bacterial cell division and ultimately leads to bacterial death.
Mechanism of Action Details
Specifically, ciprofloxacin binds to these enzymes, preventing them from supercoiling and relaxing DNA. This action disrupts the bacterial cell cycle, halting its growth and leading to cell death. The drug’s potency hinges on its ability to selectively target bacterial enzymes, leaving human enzymes largely unaffected.
Spectrum of Activity
Ciprofloxacin exhibits a broad spectrum of activity, effectively targeting many Gram-negative and some Gram-positive bacteria. However, its efficacy against MRSA is limited.
- Gram-negative bacteria: Ciprofloxacin is generally effective against Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and many others.
- Gram-positive bacteria: Activity is less consistent and often less potent. It demonstrates variable activity against Staphylococcus aureus, with resistance being a significant concern, especially with MRSA.
MRSA Considerations
The development of resistance mechanisms in S. aureus, including mutations in the target enzymes (gyrase and topoisomerase IV), significantly reduces ciprofloxacin’s effectiveness against MRSA. Therefore, ciprofloxacin should not be considered a first-line treatment for MRSA infections. Alternative antibiotics with proven activity against MRSA are preferred. Always consult a physician for appropriate antibiotic selection.
Factors Influencing Activity
- Bacterial species: Inherent susceptibility varies significantly between bacterial species.
- Antibiotic concentration: Higher concentrations generally improve efficacy but are limited by toxicity.
- Resistance mechanisms: Mutations and efflux pumps significantly impact the effectiveness of ciprofloxacin.
Efficacy of Ciprofloxacin against MRSA: Clinical Evidence
Ciprofloxacin’s effectiveness against methicillin-resistant Staphylococcus aureus (MRSA) is limited. It’s crucial to understand this before considering it as a treatment option.
Most MRSA strains exhibit resistance to fluoroquinolones, the class of antibiotics to which ciprofloxacin belongs. This resistance stems from mutations in the bacterial DNA gyrase and topoisomerase IV enzymes, targets of ciprofloxacin’s action.
- Studies consistently show low susceptibility rates of MRSA to ciprofloxacin. Specific percentages vary based on geographic location and time period, but generally fall well below the threshold for effective treatment.
- Clinical trials rarely demonstrate ciprofloxacin’s success against MRSA infections. Alternatives consistently show superior outcomes.
- Laboratory susceptibility testing is essential before considering ciprofloxacin for any infection. However, even if in vitro testing suggests susceptibility, clinical success remains unlikely due to the complex nature of infection and the high probability of resistance.
Instead of ciprofloxacin, clinicians typically choose antibiotics with proven activity against MRSA. These include:
- Vancomycin
- Daptomycin
- Linezolid
- Ceftaroline
- Telavancin
The choice depends on factors such as infection site, patient history, and local resistance patterns. Always consult current treatment guidelines and local antibiograms for the most up-to-date recommendations. Prescribing ciprofloxacin for MRSA is generally discouraged due to the high likelihood of treatment failure and potential contribution to further antimicrobial resistance.
Limitations of Ciprofloxacin in Treating MRSA Infections
Ciprofloxacin, a fluoroquinolone antibiotic, is generally ineffective against methicillin-resistant Staphylococcus aureus (MRSA) infections. MRSA bacteria possess altered penicillin-binding proteins, rendering them resistant to many beta-lactam antibiotics, including methicillin. This resistance mechanism frequently extends to fluoroquinolones like ciprofloxacin. Laboratory testing often shows minimal inhibitory concentrations (MICs) far exceeding achievable therapeutic levels in the body.
Resistance Mechanisms
MRSA develops resistance via mutations in its DNA gyrase and topoisomerase IV genes. These enzymes are crucial targets of fluoroquinolones. Mutations result in decreased drug binding, hindering ciprofloxacin’s ability to inhibit bacterial DNA replication and repair, thus promoting bacterial survival and proliferation. The spread of resistance genes via plasmids further complicates treatment.
Clinical Implications
Using ciprofloxacin to treat MRSA infections is unlikely to yield positive results. It may even contribute to the development of further antibiotic resistance. This can lead to prolonged illness, increased risk of complications, and a need for more potent, and potentially more toxic, treatment options. Always rely on culture and sensitivity testing to guide antibiotic choices; ciprofloxacin should only be considered for MRSA if testing specifically demonstrates susceptibility.
Alternative Treatment Options for MRSA Infections
MRSA infections often require treatments beyond Ciprofloxacin. Clinicians frequently prescribe daptomycin, vancomycin, or linezolid as first-line alternatives depending on the infection site and severity. These drugs directly target bacterial cell walls or protein synthesis, effectively combating MRSA.
Surgical Debridement and Drainage
For localized MRSA infections like abscesses, surgical intervention is key. This involves draining pus and removing infected tissue, promoting healing and reducing the bacterial load. This procedure often complements antibiotic therapy.
Other Antibiotic Options
Telavancin, ceftaroline, and tigecycline represent further antibiotic choices. However, their use should be guided by susceptibility testing and consideration of potential side effects. These antibiotics employ different mechanisms to inhibit bacterial growth or kill bacteria. Always consult a physician for appropriate treatment selection.
When to Consider Ciprofloxacin for MRSA-Related Conditions
Ciprofloxacin, a fluoroquinolone antibiotic, is not a first-line treatment for MRSA infections. Its use should be reserved for specific circumstances guided by antibiotic susceptibility testing and clinical judgment.
Consider Ciprofloxacin only after other appropriate antibiotics, such as vancomycin or linezolid, have failed or are contraindicated. This is particularly relevant in cases of:
| Condition | Reason for Ciprofloxacin Consideration |
|---|---|
| MRSA Skin Infections (with specific susceptibility) | If the MRSA strain demonstrates in vitro susceptibility to Ciprofloxacin and other, safer options are ineffective or intolerable. Always prioritize less toxic alternatives. |
| Certain Gastrointestinal Infections (with specific susceptibility) | In situations where MRSA is causing a gastrointestinal infection and the strain shows susceptibility to Ciprofloxacin, and other treatments are unsuitable. This is rare. |
| Prophylaxis in Specific High-Risk Situations (under strict guidance) | Extremely limited circumstances, such as a confirmed exposure to a Ciprofloxacin-susceptible MRSA strain, might warrant prophylactic use; however, this should only be determined by an infectious disease specialist after careful risk-benefit assessment. Alternatives are usually preferred. |
Remember, Ciprofloxacin use carries potential side effects. Always discuss treatment options with your doctor. They will consider your individual medical history and the results of lab tests to determine the best course of action.
Preventing MRSA Infections and the Role of Antibiotic Stewardship
Wash your hands frequently with soap and water, especially after contact with potentially contaminated surfaces or individuals. This simple act significantly reduces MRSA transmission.
Avoid sharing personal items like towels, razors, and clothing. MRSA thrives in moist environments and can easily spread through contact.
Keep wounds clean and covered. Proper wound care prevents bacteria from entering the body and causing infection.
Antibiotic Stewardship: Your Role
Only take antibiotics prescribed by a doctor for a bacterial infection. Antibiotics are ineffective against viral infections like the common cold or flu, and overuse contributes to antibiotic resistance.
Complete the entire course of antibiotics, even if you start feeling better. Stopping early allows resistant bacteria to survive and multiply.
Never share or save antibiotics for later use. Antibiotics should be tailored to specific infections, and improper use can be harmful.
If you have MRSA, follow your doctor’s treatment plan precisely. This ensures the most effective outcome and limits further spread.
Hospital and Healthcare Settings
Healthcare facilities play a vital part in infection control. They implement strict hygiene protocols, including hand hygiene, isolation precautions for infected patients, and environmental cleaning.
Reporting suspected MRSA infections promptly allows for timely intervention and prevents outbreaks. Early detection and appropriate measures greatly reduce transmission within healthcare settings.