If you have an amoxicillin allergy, you need to know about potential cross-reactivity with other penicillin-based antibiotics. This means your allergy might extend to similar drugs, causing similar reactions. Approximately 10% of individuals reporting penicillin allergy experience cross-reactivity.
Understanding the specific penicillin structure is key. Amoxicillin belongs to the aminopenicillin group. Cross-reactivity is most likely with other aminopenicillins (like ampicillin) and, to a lesser extent, with other penicillin classes (e.g., penicillin G, methicillin). Cephalosporins, sharing structural similarities, pose a risk, although the probability is lower, generally estimated at 1-7%.
Always inform your doctor about all your allergies, including the specifics of your amoxicillin reaction (rash, hives, anaphylaxis, etc.). This detailed information allows for safer antibiotic selection. Avoid self-medicating; a physician can assess your allergy history and prescribe an appropriate alternative, such as macrolides (erythromycin, azithromycin) or tetracyclines, if needed. Remember, accurate diagnosis and informed medication choices minimize risks.
Specific reactions vary. A mild rash from amoxicillin doesn’t automatically mean severe reactions to other penicillins. However, a history of anaphylaxis demands extreme caution and necessitates careful consideration when prescribing any penicillin-related drug. A skin prick test or blood test can aid in determining your specific sensitivities and guide treatment strategies.
- Amoxicillin Allergy Cross-Reactivity: A Detailed Overview
- Understanding Amoxicillin’s Chemical Structure and Allergic Reactions
- Common Cross-Reactive Antibiotics: Identifying Potential Triggers
- Other Potential Cross-Reactive Drugs
- Symptoms of Amoxicillin Allergy and Cross-Reactivity: Recognizing the Signs
- Testing for Amoxicillin Allergy and Cross-Reactivity: Diagnostic Procedures
- Specific IgE Blood Tests
- Oral Challenge Testing
- Management of Amoxicillin Allergy and Cross-Reactive Reactions: Treatment Strategies
- Alternative Antibiotics
- Managing Cross-Reactivity
- Desensitization
- Treatment Summary Table
- Additional Considerations
- Safe Antibiotic Alternatives for Patients with Amoxicillin Allergy: Avoiding Cross-Reactions
- Living with Amoxicillin Allergy: Practical Advice and Precautions
- Understanding Cross-Reactivity
- Managing Reactions
Amoxicillin Allergy Cross-Reactivity: A Detailed Overview
Consult your doctor immediately if you suspect an amoxicillin allergy. Accurate diagnosis is paramount for safe treatment.
Amoxicillin belongs to the penicillin family of antibiotics. Cross-reactivity means an allergy to one penicillin can trigger reactions to others. This is because these antibiotics share similar chemical structures, causing your immune system to recognize them as similar threats.
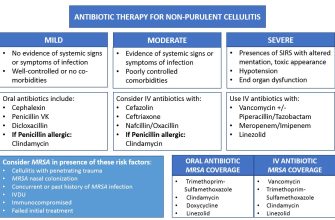
- Penicillins with high cross-reactivity: Ampicillin, methicillin, and piperacillin share significant structural similarities and are most likely to cause reactions in individuals allergic to amoxicillin.
- Penicillins with moderate cross-reactivity: Dicloxacillin, nafcillin, and oxacillin have some structural similarities but may not always trigger a reaction.
- Cephalosporins: These are a related class of antibiotics. While not always causing reactions, a percentage of those allergic to penicillins experience cross-reactivity with cephalosporins. Your doctor will assess your individual risk.
The severity of cross-reactivity varies widely. Reactions can range from mild skin rashes to life-threatening anaphylaxis. A history of severe penicillin allergy necessitates careful medical evaluation before prescribing any related antibiotic.
- Skin testing: This can identify specific allergens and guide treatment decisions.
- Detailed medical history: This includes the type of reaction, its severity, and any prior experiences with other antibiotics.
- Careful medication selection: Alternatives exist, such as macrolides, tetracyclines, or fluoroquinolones, depending on the infection.
Accurate allergy information is crucial. Always inform all your healthcare providers about any known drug allergies. This will ensure safe and effective medical care.
Remember: This information is for educational purposes only and does not substitute professional medical advice. Always seek guidance from a qualified healthcare professional for diagnosis and treatment.
Understanding Amoxicillin’s Chemical Structure and Allergic Reactions
Amoxicillin, a penicillin-derivative, contains a β-lactam ring. This crucial structural feature is responsible for its antibacterial action, but also for its allergenic potential. The β-lactam ring interacts with specific proteins in the body, triggering an immune response in susceptible individuals.
Allergic reactions arise from the body’s recognition of amoxicillin (or its metabolites) as a foreign substance. This leads to the production of IgE antibodies. Subsequent exposure to amoxicillin causes a rapid release of histamine and other mediators, resulting in symptoms ranging from mild skin rashes to life-threatening anaphylaxis.
The specific amino acid side chain attached to the β-lactam ring modifies amoxicillin’s properties, influencing both its efficacy and allergenicity. Differences in side chains among penicillin antibiotics directly affect cross-reactivity potential.
Understanding this chemical basis is key. Amoxicillin’s structure explains why cross-reactivity with other penicillins is common. Individuals allergic to one penicillin are often allergic to others due to the shared β-lactam core.
Careful medical history and allergy testing are paramount before prescribing amoxicillin. This reduces the risk of adverse reactions. Patients with a known penicillin allergy require careful consideration for alternative antibiotic therapies.
Severe allergic reactions, such as anaphylaxis, necessitate immediate medical attention. Early recognition and treatment are vital for preventing complications.
Common Cross-Reactive Antibiotics: Identifying Potential Triggers
If you have a known amoxicillin allergy, avoid penicillin-based antibiotics like ampicillin, dicloxacillin, and piperacillin. These share a similar chemical structure and often trigger similar allergic reactions.
Cephalosporins, another class of antibiotics, also exhibit cross-reactivity with penicillins. While the risk is lower than with other penicillins, cefaclor, cefadroxil, cefazolin, and ceftriaxone should be approached cautiously. Always inform your doctor of your penicillin allergy before receiving any cephalosporin.
Other Potential Cross-Reactive Drugs
Certain carbapenems, such as imipenem and meropenem, may cause cross-reactivity in some individuals. This is less frequent than with penicillins and cephalosporins, but still warrants consideration. Your doctor will assess your risk factors.
Monobactams, like aztreonam, generally show less cross-reactivity but it still can occur. This makes them a possible alternative for those with penicillin allergies, though an allergy test is usually advisable.
Always discuss your allergy history thoroughly with your doctor or allergist before starting any antibiotic treatment. They can guide you towards safe and effective alternatives.
Symptoms of Amoxicillin Allergy and Cross-Reactivity: Recognizing the Signs
Identifying an amoxicillin allergy requires careful observation of symptoms. Reactions range in severity, from mild to life-threatening.
Mild reactions often include:
- Hives (urticaria): Raised, itchy welts on the skin.
- Itching (pruritus): Generalized or localized skin itching.
- Rash: Red, bumpy skin eruption.
- Swelling (angioedema): Swelling of the face, lips, or tongue.
Severe reactions, requiring immediate medical attention, are characterized by:
- Anaphylaxis: This is a medical emergency. Symptoms include difficulty breathing, wheezing, rapid heartbeat, dizziness, and sudden drop in blood pressure.
Cross-reactivity means your body’s immune system might react to other penicillin-like antibiotics after an amoxicillin allergy. These include:
- Ampicillin
- Dicloxacillin
- Piperacillin
- Cefazolin (a cephalosporin – a related class of antibiotics)
Symptoms of cross-reactivity mirror those of amoxicillin allergy, ranging from mild skin reactions to life-threatening anaphylaxis. The severity can vary between individuals and even across different exposures to the same medication.
If you experience any of these symptoms after taking amoxicillin or a similar antibiotic, seek medical help immediately. Early intervention is vital to managing allergic reactions and preventing serious complications.
Testing for Amoxicillin Allergy and Cross-Reactivity: Diagnostic Procedures
Skin prick tests are the primary method for diagnosing amoxicillin allergy. A small amount of amoxicillin is applied to your skin, and a tiny prick is made to allow the allergen to enter. A positive reaction, indicated by a wheal (raised bump) and flare (redness), suggests allergy. A negative result, however, doesn’t definitively rule out allergy; some individuals may have a negative skin test yet still experience a reaction.
Specific IgE Blood Tests
Specific IgE blood tests measure the levels of IgE antibodies specific to amoxicillin in your blood. Elevated levels suggest an allergic sensitization. This test is particularly useful for patients with severe eczema or other skin conditions that can interfere with skin prick testing. It’s important to note that a positive result doesn’t always correlate with clinical allergy; a careful clinical history remains crucial.
Oral Challenge Testing
This involves carefully controlled ingestion of increasing doses of amoxicillin under medical supervision. This is the gold standard for confirming allergy, but it’s risky and should only be done when the potential benefits outweigh the risks of a reaction. It’s primarily used to confirm a true allergy in patients with a negative skin prick test or when cross-reactivity needs precise determination.
Remember to discuss all testing options with your doctor to determine the most appropriate approach given your individual circumstances and medical history. Accurate diagnosis is crucial for safe medication choices.
Management of Amoxicillin Allergy and Cross-Reactive Reactions: Treatment Strategies
First, accurately determine the nature of the reaction. A true allergy requires a detailed history and possibly allergy testing. Mild reactions, like hives, often respond well to antihistamines like diphenhydramine (Benadryl) or cetirizine (Zyrtec). For more severe reactions, such as angioedema or anaphylaxis, immediate medical attention is crucial, involving epinephrine injection and supportive care.
Alternative Antibiotics
If amoxicillin is contraindicated, select an alternative antibiotic from a different class. Cephalosporins, though structurally related to penicillins, might still trigger a reaction in some patients; careful assessment is needed. Good alternatives include azithromycin, clarithromycin (macrolides), or trimethoprim-sulfamethoxazole (TMP-SMX) – each with its own potential side effects and contraindications. Always consider the specific infection and patient factors when choosing.
Managing Cross-Reactivity
Cross-reactivity among penicillins is common. If a patient has a penicillin allergy, carefully consider the possibility of reactions to other beta-lactam antibiotics, such as cephalosporins, carbapenems, and monobactams. Skin testing can help assess the risk of cross-reactivity, but it’s not always definitive.
Desensitization
In situations where alternative antibiotics are unsuitable, desensitization may be considered. This involves gradually increasing doses of the antibiotic under close medical supervision in a controlled environment, aiming to induce tolerance. It’s a specialized procedure requiring experienced clinicians. However, success is not guaranteed, and monitoring for adverse effects is continuous throughout the process.
Treatment Summary Table
| Reaction Severity | Treatment |
|---|---|
| Mild (Hives) | Oral antihistamines (diphenhydramine, cetirizine) |
| Moderate (Angioedema) | Oral and/or injectable corticosteroids, antihistamines |
| Severe (Anaphylaxis) | Epinephrine injection, airway management, supportive care |
Additional Considerations
Patient education regarding allergy symptoms, avoidance strategies, and emergency action plans is critical. A clear medical record documenting allergy history and management is essential for future care. Regular follow-up with an allergist or physician is recommended to monitor the patient’s condition and adjust treatment as needed.
Safe Antibiotic Alternatives for Patients with Amoxicillin Allergy: Avoiding Cross-Reactions
If you have an amoxicillin allergy, your doctor will likely prescribe an alternative. Common choices include cephalosporins, macrolides, and fluoroquinolones. However, cross-reactivity exists. Approximately 10% of individuals with penicillin allergy will also react to cephalosporins. This percentage varies based on the specific cephalosporin and the nature of the penicillin allergy.
Cephalosporins: While cross-reactivity is possible, patients with mild amoxicillin reactions often tolerate cephalosporins. Ceftriaxone and cefazolin are often safer alternatives than cefalexin or cefuroxime. Always inform your doctor of your allergy history to ensure appropriate selection.
Macrolides: Azithromycin and erythromycin are frequently used alternatives. These antibiotics work differently than penicillins and cephalosporins, reducing cross-reactivity risk. However, macrolides can cause gastrointestinal upset in some individuals.
Fluoroquinolones: Ciprofloxacin and levofloxacin provide another option. They possess a distinct chemical structure from penicillin and have a low risk of cross-reactivity. However, fluoroquinolones carry a risk of tendinitis and tendon rupture, particularly in older adults.
Other options: Depending on the infection, your doctor might consider tetracyclines (e.g., doxycycline, minocycline), clindamycin, or linezolid. These are often reserved for specific infections and might have side effects unique to them.
Before starting any antibiotic, always discuss your medical history and allergy details with your physician to choose the safest and most effective treatment. Allergy testing can provide further clarification about the severity and specifics of your allergy.
Living with Amoxicillin Allergy: Practical Advice and Precautions
Always carry your allergy information. Include your diagnosis, the reaction you experienced, and any alternative medications your doctor has prescribed. A medical alert bracelet or necklace is also highly recommended.
Inform all your healthcare providers – doctors, dentists, and even pharmacists – about your allergy. This includes providing them with a copy of your allergy details. Don’t hesitate to ask questions about any medications they plan to prescribe.
Understanding Cross-Reactivity
Amoxicillin belongs to the penicillin family. Be aware of potential cross-reactivity with other penicillins like ampicillin and piperacillin. Discuss alternative antibiotics with your physician if a penicillin-based medication is suggested. Some individuals allergic to penicillin may also react to cephalosporins.
Always read medication labels carefully. Many over-the-counter products contain amoxicillin or other related substances. Check labels for hidden ingredients. This vigilance applies to cold medications, pain relievers, and even some topical creams.
Managing Reactions
Know the signs of your allergic reaction. This could range from mild skin rashes to severe anaphylaxis. Have an action plan ready, including knowing when to use an epinephrine auto-injector (if prescribed) and when to seek immediate medical attention. Discuss this plan with your doctor to ensure it’s tailored to your specific needs.
Carry an emergency kit. This should contain your epinephrine auto-injector (if prescribed), antihistamines, and your allergy information card. Keep your kit readily accessible at all times.