If you have a known allergy to amoxicillin, several alternatives can safely replace this antibiotic for treating infections. Consider options like cefuroxime, which belongs to the cephalosporin class and is effective against a range of bacterial infections. Your healthcare provider may recommend this based on your specific condition and history.
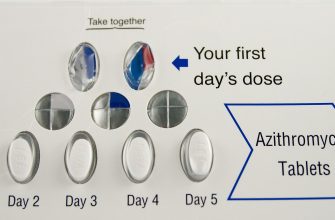
Azithromycin is another excellent choice, particularly for respiratory infections. It operates differently than amoxicillin, making it suitable for individuals who experience allergic reactions to penicillin-based drugs. Always discuss with your doctor to ensure it suits your needs and won’t interact with any other medications you are taking.
If you face difficulty tolerating oral antibiotics, clindamycin may be prescribed. This alternative is effective against similar infections while being a good option for those with penicillin allergies. Keep in mind that clindamycin is often used for skin infections and certain dental concerns.
For urinary tract infections, consider nitrofurantoin or trimethoprim-sulfamethoxazole, which are both well-tolerated in patients who cannot take amoxicillin. Discuss these options with your healthcare provider to find the best fit for your medical history.
Lastly, always communicate your allergy status to your healthcare team. Monitoring for any adverse reactions, regardless of the alternative chosen, ensures safe and effective treatment tailored to your health needs.
- Allergy to Amoxicillin Alternatives
- Understanding Amoxicillin Allergy Symptoms
- Mild Symptoms
- Severe Symptoms
- Diagnosis: How to Identify Amoxicillin Allergy
- Alternative Antibiotics for Bacterial Infections
- Considerations for Choosing Alternatives to Amoxicillin
- Non-Antibiotic Alternatives for Treating Infections
- Honey and Its Healing Properties
- Essential Oils for Infection Management
- Managing Allergic Reactions to Amoxicillin Alternatives
- Consulting Healthcare Professionals: When to Seek Help
- Signs You Should Consult a Healthcare Professional
- Questions to Ask Your Healthcare Provider
- Future of Allergy Research: What’s on the Horizon?
- Immunotherapy Innovations
- Biologics and Targeted Therapies
Allergy to Amoxicillin Alternatives
If you have an allergy to amoxicillin, several alternatives can be considered for treating infections. Here are some commonly recommended options:
- Cefdinir: This cephalosporin antibiotic can treat a variety of bacterial infections.
- Cefuroxime: Another cephalosporin that is effective against respiratory tract infections.
- Doxycycline: A tetracycline antibiotic used for various infections, including respiratory and skin conditions.
- Clindamycin: This antibiotic is useful for treating certain types of skin infections and anaerobic infections.
- Azithromycin: Widely used for respiratory infections and certain sexually transmitted infections.
- Levofloxacin: A fluoroquinolone effective in treating a broad range of infections.
Consult your healthcare provider or an allergist to determine which alternative suits your needs. They will consider your medical history, severity of the allergy, and specific infection to tailor the best treatment plan for you.
Always inform healthcare professionals of any drug allergies before starting new medications. Monitor for any adverse reactions when trying a new antibiotic, and report any unusual symptoms immediately.
In cases where multiple allergies exist, a specialist may conduct an allergy testing to explore other suitable options. Personalized treatment approaches may yield the best results in managing bacterial infections safely.
Understanding Amoxicillin Allergy Symptoms
Watch for skin reactions such as hives, itching, or rashes to identify an amoxicillin allergy. These responses typically appear within hours to days after taking the medication. Severe reactions, including anaphylaxis, require immediate medical attention. Signs may include difficulty breathing, swelling of the face or throat, and a rapid heartbeat.
Mild Symptoms
Mild symptoms may consist of gastrointestinal discomfort, like nausea or vomiting, which can occur shortly after beginning the treatment. You might also experience a fever or general malaise. These signs often warrant consulting a healthcare provider to assess whether amoxicillin is the cause.
Severe Symptoms
Severe allergic reactions necessitate urgent care. Symptoms like swelling, especially around the eyes and lips, or difficulty swallowing can signify a serious condition. If you encounter these reactions, seek emergency medical help immediately. Keeping a list of any allergies and discussing it with healthcare professionals ensures safer treatment plans in the future.
Diagnosis: How to Identify Amoxicillin Allergy
Begin by assessing symptoms after amoxicillin intake. Common reactions include skin rashes, itching, hives, and swelling. Immediate evaluation is necessary for severe reactions such as difficulty breathing or anaphylaxis. Record the timing and nature of symptoms to provide accurate information to healthcare providers.
Consult a healthcare professional who can perform skin tests. These tests help determine allergic reactions to penicillin and its derivatives, including amoxicillin. A negative skin test generally indicates a low likelihood of allergy.
In some cases, an oral challenge may be necessary. This involves administering a small dose of amoxicillin under medical supervision to monitor for allergic reactions. Ensure the patient is in a controlled environment, as this procedure can trigger responses.
Keep track of any other medications or allergies. History of reactions to penicillins, cephalosporins, or other antibiotics increases the likelihood of amoxicillin allergy. Document previous allergic reactions and communicate this information during medical consultations.
| Symptom | Timing |
|---|---|
| Skin rash | Within hours to days |
| Itching | Minutes to days |
| Hives | Immediate to hours |
| Swelling | Minutes to hours |
| Difficulty breathing | Immediate |
Maintain open communication with your healthcare provider to ensure accurate diagnosis and management. Misdiagnosis can lead to incorrect medication prescriptions. Be proactive in discussing concerns about amoxicillin and exploring alternative treatments if needed.
Alternative Antibiotics for Bacterial Infections
Consider using the following antibiotics if you are allergic to amoxicillin:
- Ciprofloxacin: This fluoroquinolone antibiotic treats a variety of bacterial infections, especially in the urinary tract and respiratory system.
- Doxycycline: Commonly prescribed for respiratory infections, acne, and certain sexually transmitted infections, this tetracycline works effectively against different bacteria.
- Levofloxacin: Another fluoroquinolone, levofloxacin is effective for pneumonia, sinusitis, and skin infections.
- Clindamycin: This lincosamide antibiotic is effective for treating skin infections and certain respiratory infections, especially when penicillins are not suitable.
- Azithromycin: Widely used for respiratory tract infections and STIs, azithromycin is a macrolide antibiotic that provides broader coverage against many bacteria.
Always consult your healthcare provider before starting any new medication. They can suggest the most appropriate alternative based on your specific condition and medical history.
For patients with specific infections, consider the following:
- Upper Respiratory Infections: Azithromycin or doxycycline can be effective choices.
- Skin Infections: Clindamycin or doxycycline provide good coverage and may be preferred.
- Urinary Tract Infections: Ciprofloxacin is often recommended, but levofloxacin can also be a suitable option.
Monitoring for potential side effects is important when using any antibiotic. Stay informed and communicate with your healthcare provider to ensure the best treatment for your infection.
Considerations for Choosing Alternatives to Amoxicillin
Evaluate the specific type of infection to choose the right alternative. Different conditions may require targeted antibiotics. For instance, penicillin allergies often lead healthcare providers to prescribe alternatives such as cephalexin or clindamycin for skin or respiratory infections.
Review the patient’s medical history carefully. Past reactions to medications can guide the choice of alternatives. If a patient exhibits allergy symptoms to penicillin-class antibiotics, alternatives should fall outside this category to avoid cross-reactivity.
Assess the spectrum of activity of potential substitutes. Some antibiotics have broader activity against bacteria, while others target specific strains. Consider the susceptibility pattern of the pathogens involved to ensure efficacy.
Consult with an infectious disease specialist if there are doubts about appropriate alternatives. Their expertise can provide insights into lesser-known options or newer antibiotics that might suit particular cases.
Factor in side effect profiles of alternatives. Some antibiotics are associated with gastrointestinal disturbances, while others might lead to more severe adverse effects. Balancing the potential risks against the benefits is crucial in decision-making.
Discuss with the patient about the alternatives, including potential side effects and expected outcomes. This open communication helps in building trust and encourages adherence to the treatment plan.
Monitor the patient closely after initiating alternative therapy. Adjustments may be necessary based on the individual’s response or development of any unexpected complications. Continuous evaluation supports the best treatment outcomes.
Non-Antibiotic Alternatives for Treating Infections
Consider using probiotics to enhance gut health and support the immune system during an infection. Probiotics can help restore the balance of beneficial bacteria, which can be disrupted during illness. Look for strains like Lactobacillus and Bifidobacterium, often found in yogurt and supplements.
Other potential options include herbal remedies such as garlic, which possesses natural antimicrobial properties. Incorporating garlic into your diet may help combat infections without the use of antibiotics. Turmeric, known for its anti-inflammatory characteristics, can also aid in reducing infection-related inflammation. Add turmeric to meals or consume it as a supplement to reap its benefits.
Honey and Its Healing Properties
Honey has been recognized for its wound-healing and antibacterial effects. Applying raw honey topically to minor wounds can help prevent infection. Consuming honey can also soothe a sore throat and reduce coughing, providing symptomatic relief.
Essential Oils for Infection Management
Essential oils like tea tree oil and oregano oil offer additional alternatives. Tea tree oil can be diluted and used topically for skin infections, while oregano oil may be taken in capsule form to support immune function. Always ensure these oils are properly diluted and consult a healthcare provider before use.
Managing Allergic Reactions to Amoxicillin Alternatives
Identify the symptoms of an allergic reaction such as rashes, itching, or swelling. If these occur after taking an alternative, stop using the medication immediately.
- Consult your healthcare provider: Discuss any observed reactions. They may recommend allergy testing or alternative antibiotics.
- Use antihistamines: Over-the-counter antihistamines can help alleviate mild allergic symptoms. Always consult a physician for dosages and recommendations.
- Maintain a medication diary: Keep track of all medications taken and any reactions noted. This information aids healthcare professionals in creating a safe treatment plan.
If a severe allergic reaction occurs, use an epinephrine auto-injector if prescribed, and seek emergency medical help immediately.
- Alternative antibiotics: Discuss options like azithromycin or clindamycin with your doctor.
- Non-antibiotic options: For non-bacterial conditions, consider alternative treatments as suggested by your healthcare provider.
- Education: Learn about potential allergens and communicate with all healthcare providers to avoid future incidents.
Monitoring symptoms closely and timely interventions can significantly reduce risks associated with allergic reactions. Create a proactive plan with your healthcare team for safe medication management.
Consulting Healthcare Professionals: When to Seek Help
If you have a confirmed allergy to amoxicillin and require alternative treatments, consulting a healthcare professional becomes imperative. Schedule an appointment if you experience adverse reactions from medications or have a history of severe allergies. Early intervention can prevent complications and ensure appropriate care.
Signs You Should Consult a Healthcare Professional
Pay attention to the following signs:
- Symptoms of a severe allergic reaction, such as difficulty breathing, swelling of the face or throat, or rapid heartbeat.
- Persistent skin rashes, itching, or hives after taking a new antibiotic.
- New or unusual symptoms following medication use that may indicate an allergic response.
Questions to Ask Your Healthcare Provider
When you meet with your healthcare provider, consider asking:
- What alternative medications are available for my condition?
- Are there specific tests to evaluate my allergy to amoxicillin and similar antibiotics?
- What should I do if I experience an allergic reaction to a prescribed medication?
| Symptom | Action |
|---|---|
| Shortness of breath | Seek emergency care immediately |
| Severe rash or hives | Contact your healthcare provider for evaluation |
| Unexplained symptoms | Document and discuss during your next appointment |
Engaging with a healthcare professional ensures the selection of a safe and effective treatment plan while considering your allergies. Keep an open line of communication and advocate for your health needs. Taking these proactive steps helps manage your allergies and supports your overall well-being.
Future of Allergy Research: What’s on the Horizon?
Personalized medicine is reshaping allergy treatment. Advances in genetic research allow for tailored therapies that suit individual patient profiles. Understanding genetic markers linked to allergies can help identify those at risk and determine the most effective treatments.
Immunotherapy Innovations
Recent developments in immunotherapy show promise for treating amoxicillin allergies. Subcutaneous and sublingual immunotherapy options are expanding, offering new avenues for desensitization. Research is ongoing into orally administered therapies that may provide safer and more convenient options.
Biologics and Targeted Therapies
Biologic agents, targeting specific pathways in the immune response, present exciting possibilities for allergic reactions. Current studies focus on monoclonal antibodies that inhibit IgE production or block its action, enhancing safety and effectiveness. These treatments aim to reduce allergic symptoms without the need for broad-spectrum antibiotics.